Degenerative Adult Scoliosis FAQs
What is degenerative scoliosis ?
Written By DR CHOW Hung-Tsan
(Last updated on: September 15th 2020)
Degenerative lumbar scoliosis (Fig. 1) is a side deviation of the spine that is common in the elderly population. In terms of objective measurement, it is defined as a spinal deformity in a skeletally mature patient with a Cobb angle of more than 10° in the coronal plain 4, 11, 12. Primary degenerative scoliosis or “De Novo” scoliosis is a deformity developing in a previously straight spine, caused by accelerated degeneration of the spine in middle age with progressive disc.
 |
| Fig 1. Degenerative Lumbar Scoliosis |
How common is the degenerative scoliosis ?
There is no real figure in Hong Kong. There is an increase trend of the incidence in our practice and required treatment. The prevalence of degenerative scoliosis can be up to 68% of the population in developed countries 1, 2, 6–10.
How many types of degenerative scoliosis ?
Aebi 2015 classified adult scoliosis into three major types 4. Type I scoliosis is the primary degenerative or de novo scoliosis which develops after skeletal maturity and is characterised by minimal structural vertebral deformities, advanced degenerative changes, and a predominance of lower lumbar curves.
Type II scoliosis is the progressive idiopathic deformity that develops before skeletal maturity but becomes symptomatic in adult life.
Type III Secondary Degenerative Scoliosis
Scoliosis following idiopathic or other forms of scoliosis or occurring in the context of a pelvic obliquity due to a leg-length discrepancy, hip pathology, or a lumbosacral transitional anomaly, mostly located in the thoraco-lumbar, lumbar, or lumbosacral.
Scoliosis secondary to metabolic bone disease (mostly osteoporosis) combined witasymmetric arthritic dis- ease and/or vertebral fractures 4.
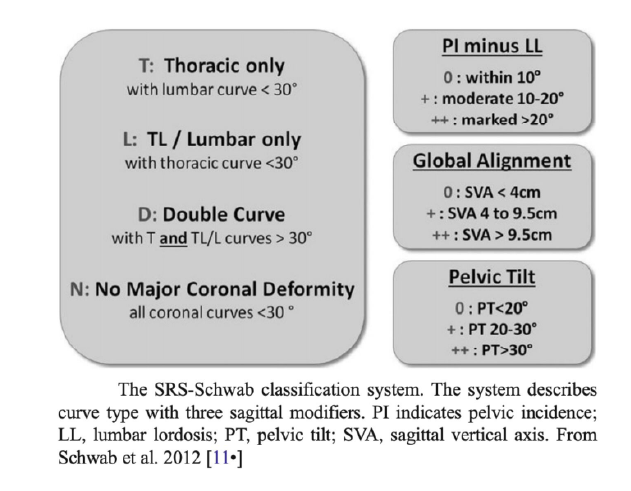 |
Fig 2. SRS- Schwab’s classification: 2012 (14) |
What cause the degenerative scoliosis ?
Although the aetiology is unclear, it is likely related to progressive and asymmetric degeneration of the disc, facet joints, and other structural spinal elements typically leading to neural element compression.
It is a difficult disease in terms of treatment because of perioperative morbidity, lack of powerful instrumentation, high incidence of neurological deficit, and relative rigidity of the deformity, the risk–benefit curve in the treatment of adults with scoliosis usually tilted towards non-operative treatment such as anti-inflammatory, muscle relaxant, pain killers, physical therapy etc.
With advancement of surgical techniques and instrumentation, there is a significant evolution of the management of this problem during the past decade. This has been supported with the multidisciplinary progress in anaesthesia for spinal surgery and radiology by more sophisticated and precise diagnostic imaging and differentiated application of invasive and functional diagnostic tests.
Increased in the demand for the surgical treatment as patient more aware of the importance of quality of life and less acceptance to functional limitations in their adult deformity 6.
What are the symptoms ?
Slowly progressive low back pain is the commonest symptoms. A small proportion of patient came to see their spine surgeon complaining their progressive spinal deformity. The symptoms are usually mild at the beginning until there is some complications happen to make the pain more severe to them. Neurological symptoms (such as leg pain, sciatica, lower limb numbness) are common by the time when they go to see their doctor. Lower limb sensory loss or even weakness may happen if the early symptoms being neglected. In the worse case scenario, patient can have bowel and bladder control failure or even paralysis.
What clinical assessment is necessary ?
The first step is to take a medical history such as the primary symptoms of the lower back, the history of the deformity of the lower back, functional loss affecting the daily living, any family history of scoliosis, neurological symptoms include muscle weakness, sensation loss and spinster dysfunction. Previous history of any spine surgery and other medical conditions are crucial for the decision of the treatment.
Clinical assessment start with general assessment such as gait assessment, posture on standing, and bending movement of the body. This give us a general idea of how severe is problem affecting their daily lives. Specific examinations include measurement of the leg length, measuring the rib hump, flexibility of the curves, any lower limb neurological dysfunction. Occasionally, we will need to check the sphincter functions by digital rectal examination.
 |
| Fig 3. Kyphotic Deformity |
What X ray can tell us ?
X-rays allow us to see the structure of the spine and measure the curves.
Basic X rays include standing whole spine AP and Lateral view (Fig 4). Usually, your doctor will measure the angles of the curves that is Cobb’s angle. Lateral view is able to see the lumbosacral alignment. Pelvic Incidence is the angle which is a guide for your normal lumbar lordosis angle.
Standing lateral flexion/extension are important to see any instability and the range of motion of the lower back.
Supine side bending AP views are able to see the reducibility of the curve if surgery is considered. Sequential X rays at different stage may be necessary to assess the progression of the curve. Any past X-rays taken of your spine can be very helpful to your spine surgeon.
 |
| Fig 4. X-ray whole Spine AP/LAT on Standing |
Any other imaging is necessary ?
MRI scan (Fig 5) lumbar spine is required to look for any spinal cord compression or nerve root compression. Spinal stenosis is the most commonest associated pathology leading to pain and/or lower limb neurological symptoms. It is the commonest reason to bring the patient to the spine surgeon.
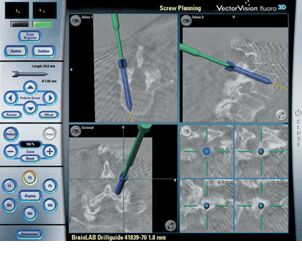
Computerised Tomogram (CT) scan is necessary if decided for surgical treatment an occasionally need in the follow up. It is very helpful for pre-operative planning of the surgical steps and implant size templating.
By reconstructing the images, we can see the deformity in 3 dimensional way. The data from CT scan can also be used in navigation machine to guide us the direction of the screw fixation during the surgery. (Fig 6)
In the follow up, we might need CT scan to assess the fusion status which is usually happened in 9-12 months after the primary surgery.
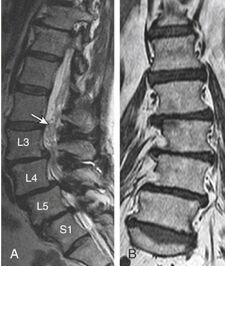 |  |
| Fig 5 MRI Scan | Fig 6. CT Scan |
What conservative treatment are available for degenerative scoliosis ?
support the spine. Mild pain medications may be recommended for use when needed. Strong pain medications, such as narcotics, are not recommended due to the risk of addiction.
Medical treatment
Oral anti-inflammatory and Neuropathic pain medications (e.g. Gabapentin, Pre-garbalin) are adjunct to the pain medications to control the arthritis symptoms and nerve pain 4.
If osteoporosis is present, then treatment of the osteoporosis may slow the progression of the scoliosis as well. This can be accomplished in several ways. The current recommendations include weight-bearing exercises, Calcium and vitamin D supplement, Hormone replacement therapy, and Bisphosphonate (Fosamax, Actonel, Bonviva), and Para-thyroid hormone injection (Forteo).
Physical Therapy
It is commonly prescribed to patients with back pain due to degenerative lumbar scoliosis. It helps to relief the back pain and stiffness. Core muscle strengthening may reduce the progress of the symptoms but not the speed of the progress of the degeneration or deformity.
Spine Braces and Orthotics
The use of a spinal brace may provide some pain relief. However, in adults, it will not cause the spine to straighten. Once you have reached skeletal maturity, bracing is used for pain relief rather than prevention. If there is a difference in the length of your legs, special shoe inserts or a simple shoe lift may reduce your back pain 4.
When I will need surgery ?
Surgery is indicated if the patient failed to response to conservative treatment with persistent debilitating symptoms 3.
Lower limb neurological symptoms such as numbness, claudication (limited walking distance) and nerve pain (radiculopathy) are strong indication for surgery. These symptoms are usually related to lumbar spinal stenosis. To learn more about lumbar spinal stenosis, please refer to FAQ’s of Lumbar Spinal Stenosis.
The basic principle for treating symptomatic degenerative scoliosis includes:
- Neurological decompression
- Correction of the deformity
- Spinal fusion with posterior instrumentation
Neurological decompression means removing the pressure from the nerves or spinal cord. Standard procedure is called laminotomies or laminectomies. This procedure can be done via minimal invasive technique with small incision at around 2 cm or less. For one level surgery, it usually takes one hour to complete with 50 cc or less blood loss. The recovery time is around 2-3 weeks.
Spine fusion (connecting 2 vertebrae together) is indicated for unable and deformed spine. There are many techniques in performing lumbar spinal fusion. The latest technology specifically benefit the degenerative lumbar scoliosis are minimal invasive lateral fusion via Direct Lumbar Interbody Fusion (DLIF) (Fig 7) and Oblique Lumbar Interbody Fusion (OLIF) (Fig 8). They are small incision surgery from the left side of the abdomen to achieve correction of the scoliosis and fusing the unstable spinal segment with a large fusion cage. By distracting the lumbar disc, indirect decompression of the foramen and central spinal canal can be achieved.
%20.png?1587029112848) |
| Fig 7 Direct Lateral Lumbar Interbody Fusion or Extreme Lateral Lumbar Interbody Fusion (DLIF/XLIF) |
%20.png?1587029366000) |
Fig 8 Oblique Lumbar Interbody Fusion (OLIF) |
Long posterior instrumentation (Fig 9) for spinal fusion is necessary to correct the scoliosis deformity. It is now done under navgiation robotic guidance and neuro-monitoring. The chance of neurological injury is very remote with these technology. Therefore the recovery is smooth and easy after this surgery.
How is the outcome after the surgery ?
The overall outcome after neurological decompression is usually good. There will be 90% of the nerve symptoms resolved with the surgery. There will be dramatic improvement of the alignment after the surgery. Residual back discomfort is expected because of stiffness after long instrumentation with fusion but the overall function after surgery is very well accepted 13.
Conclusions:
Long survival in our society is inevitably producing more age related health issue. As we are more healthy and physically active, we encountered more degenerative lumbar scoliosis. It is a very major surgical challenge both the patients and the spine surgery. With the advance of technology, now we can treat this kind of pathology with much easier way. The surgical outcome and risk of the treatment is much improved.
References:
- Aebi M. The adult scoliosis. Eur Spine J 2005; 14(10):925–48. [Text Wrapping Break]
- Anasetti F, Galbusera F, Aziz HN, Bellini CM, Addis A, Villa T. et. al,. Spine stability after implantation of an interspinous device: an in vitro and finite element biomechanical study. J Neurosurg Spine 2010;13(5):568–75. [Text Wrapping Break]
- Ascani E, Bartolozzi P, Logroscino CA, Marchetti PG, Ponte A, Savini R, Travaglini F, Binazzi R, Di Silvestre M (1986) Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine 11(8):784–789
- Avraam Ploumis, MD*, Ensor E. Transfledt, MD, Francis Denis, MD Degenerative lumbar scoliosis associated with spinal stenosis. The Spine Journal 2007; 7(4):428–36
- Benner B, Ehni G. Degenerative lumbar scoliosis. Spine 1979; 4: 548 [Text Wrapping Break]
- Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: Results from the first National Health and Nutrition Examination Survey. Int J Epidemiol 1987;16:537–44.[Text Wrapping Break]
- Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ) 2003;32(2):77–82.[Text Wrapping Break]
- Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis and degenerative changes in the elderly. Spine1979; 4:542–547
- Frank Schwab, MD, Jean-Pierre Farcy, MD, Keith Bridwell, MD, Sigurd Berven, MD, Steven Glassman, MD, John Harrast, MS, William Horton, MD. A Clinical Impact Classification of Scoliosis in the Adult. Spine 2006;31(18): 2109–2114[Text Wrapping Break]
- Gelalis ID, Kang JD: Thoracic and lumbar fusions for degener- ative disorders: Rationale for selecting the appropriate fusion techniques. Orthop Clin North Am 1998;29:829–842.[Text Wrapping Break]
- Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine 2005; 30(18):2024–2029[Text Wrapping Break]
- Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003;34(2):269–79.[Text Wrapping Break]
- Charles YP, Ntilikina Y. Scoliosis surgery in adulthood: what challenges for what outcome? Ann Transl Med. 2020 Jan;8(2):34. doi: 10.21037/atm.2019.10.67. Review.
- Schwab FJ, Lafage V, Shaffrey CI, Smith JS, Moal B, Klineberg EO, Ames CP, Hostin R, Fu K-MG, Kebaish KM, Burton DC, Akbarnia BA, Gupta MC, Deviren V, Mundis GM, Boachie-Adjei O, Hart RA, Bess RS. The Schwab-SRS adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Spine J. 2012;12:S18.
Articles written/edited/reviewed by Doctors of Asia Medical Specialists ©2020 Asia Medical Specialists Limited. All rights reserved. |
