Ankle Sprain FAQs
Ankle Sprain FAQs
What is an ankle sprain?
A sprain is a tear of a ligament. Ligaments are the tough fibrous tissues that connect the bones together across a joint. Ligament tears can vary from very minor - a few fibres stretched - to complete tears of the entire ligament. The most common type of sprain is a lateral ankle sprain, where the ligaments on the outer part of the ankle joint are sprained. Less common are sprains of the medial (deltoid) ligament on the inside of the joint, and sprains of the syndesmosis, which holds the tibia and fibula bones of the lower leg together, and are also known as 'high ankle sprains'.
These FAQs apply to lateral and medial ankle ligament sprains, but not to syndesmosis (high) ankle sprains, which are treated differently.
How are ankle sprains diagnosed?
History: Usually one knows one has twisted one’s ankle, and can often describe which way it twisted, but in some circumstances, such as a road accident, one may not know happened, just that it hurts.
Examination: The ligaments may be tender. The ankle may be swollen. The ligaments may be obviously loose, or the pain may cause muscle spasm which hides any looseness.
X-ray: is recommended if there is severe swelling or tenderness of the bones suggesting a fracture (Fig. 1). By following the ‘Ottawa Ankle Rules’ one can decide whether an X-ray is needed.
 Fig. 1 Normal ankle X-ray |
MRI: is recommended if there is severe swelling suggesting damage to the articular cartilage of the joint surfaces, but, apart from looking for articular cartilage damage, MRI does not help to predict which ankle sprains will get better with physiotherapy and which will require an operation, so is not routinely used to investigate acute ankle sprains [1].
What is the treatment?
'First Aid' treatment is known as 'RICE' - Rest, Ice, Compression and Elevation - all intended to reduce pain and swelling.
It is helpful to take an anti-inflammatory painkiller, such as ibuprofen (Nurofen or Advil) or one of the newer longer acting drugs regularly.
The most recent study suggests that a period of 10 days in a cast speeds recovery in grade II and III sprains, with a definite improvement relative to other treatments at 3 months, but no long-term difference. The second-best treatment was bracing. ‘Walkers’ and compression bandaging were least effective [2]. Despite the good scientific quality of this study, it is not the last word on the management of ankle sprains [3].
Physiotherapy Rehabilitation
The most important part of treatment for ankle sprains is physiotherapist-supervised rehabilitation to restore strength and balance. When the ankle is injured the muscles become both weak and, because the reflexes go slow to respond. This can be improved with a graded exercise programme using balance and reaction training aids such as wobble boards (Fig. 2) and mini-trampolines. Sometimes people with many years of ankle instability from an old injury that was never properly rehabilitated can recover with a good physiotherapy programme.
 Fig. 2 Balance training on a wobble board |
How long will it take to get better?
A very minor sprain may only be sore for a few moments, whereas a severe sprain or complete tear of the ligaments may not recover at all without an operation, but it is worth trying 3 months of physiotherapist-supervised rehabilitation before saying 'this is not getting better, an operation is needed'.
What if my ankle sprain does not recover?
About 10% of severe sprains do not recover with physiotherapy. There are three common problems following an ankle sprain: instability; articular cartilage damage; and impingement, and often they occur together, but are best placed under the cover-all title of 'Ankle Instability'.
1. Instability
This is looseness of the ligaments (Fig. 3), usually beginning with a sprain, which may have been many years ago. Typically the ankle feels 'weak' and is easily sprained - sometimes only when playing sport, sometimes in everyday activities - some people sprain their ankles stepping on cracks in the pavement. The problem with instability is that repeated episodes damage the ankle joint leading to arthritis.
 Fig. 3 Stress X-ray shows ankle instability because of torn lateral ligaments |
2. Articular Cartilage Damage
The articular cartilage is the smooth low-friction 'soft bone' which covers the bone ends making up a joint - it is the bearing surface which makes a joint a joint, and not just two pieces of bone rubbing against each other. Damage to the articular cartilage is almost equivalent to 'arthritis'.
Often the articular cartilage is locally damaged (Fig. 4) during an ankle sprain as the two main bones in the ankle, the tibia (shin) and talus (in the foot) smash against each other. Localised damage is often described as an 'osteochondral lesion' (osteo = bone; chondral = cartilage) and, in its most common location on the talus, is known as an 'osteochondral lesion of the talus' or 'OLT' - you may see this term on your MRI report.
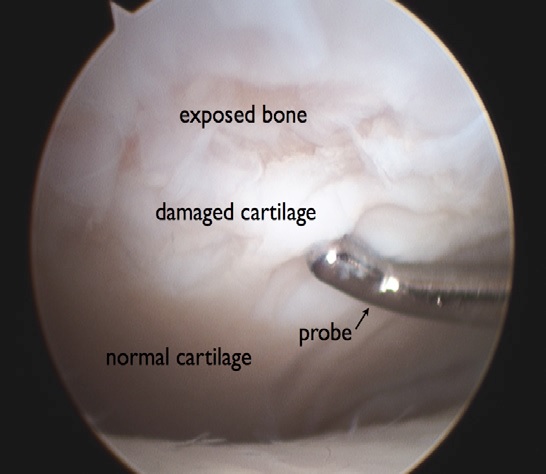 Fig. 4 Arthroscopic view of articular cartilage damage |
In time the articular cartilage damage becomes more widespread, and the ankle is described as being arthritic.
3. Impingement
Impingement means 'jamming together' and occurs when new spikes of bone (osteophytes) (Fig. 5) form along the edges of the joint, usually the front, causing pain and reducing the range of motion moving the foot up (dorsiflexion). Typically this causes pain running, especially uphill, and causes one's heel to lift up on squatting.
 Fig. 5 Extra spikes of bone in impingement |
This condition is also known as 'Footballer's Ankle' and can occur on its own without any particular injury, although it is most common in combination with ankle instability.
What is the natural history of ankle instability if left alone?
Left alone, instability usually causes arthritis of the ankle joint, possibly requiring ankle joint fusion or Total Ankle Replacement.
How is ankle instability diagnosed?
History: Most people complain of pain, swelling, giving way (or 'weak ankles') or a combination.
Examination: Often the ankle ligaments feel loose on testing, though muscle spasm can easily mask this, in impingement there is usually tenderness along the front of the ankle joint line, often with reduced range of motion, and in articular cartilage damage there may be swelling and deep tenderness.
X-rays show the extra bone in impingement, if they are taken in the right way. Sometimes this only shows up on a special anteromedial impingement view, which takes a bit of practice to get right. Established arthritis will be shown on X-ray, but subtle articular cartilage damage will not. Ligament damage or instability can be demonstrated on special stress views, but this is not usually necessary.
CT scan is helpful for showing subtle impingement and subtle bone changes underlying articular cartilage damage, but is not usually needed.
MRI shows most articular cartilage damage, and may show ligament damage - though it cannot show if the ligaments are slightly slack, and it will show other possible problems such as avascular necrosis of the talus [AVN], infection and tumour (Fig. 6).
|
Arthroscopy is the best form of diagnosis, allowing examination of the ankle ligaments without any muscle resistance while looking inside the ankle joint, and also to examine the articular cartilage with a probe - sometimes the articular cartilage is present (so it shows on the MRI), but loose (it comes away from the underlying bone when probed).
What is the treatment of these ankle problems?
Surgery
Surgery is for people who have failed to recover with physiotherapy (+/- a brace for sport) or who have impingement or significant articular cartilage damage. Usually all three instability related problems are treated together at a single operation.
Impingement
The extra bone of impingement is simply removed at arthroscopy (keyhole surgery). Two tiny holes are made in the front of the ankle joint and a small video arthroscope is placed in one and a small drill in the other and the extra bone is drilled away. This is a pretty reliable and straightforward procedure, with a quick recovery.
Articular Cartilage Damage
The treatment depends on the severity of the problem. If the damage is not too bad it might be sufficient to clean up the loose cartilage at arthroscopy - this operation is known as 'debridement' from the French. If the damage is more severe, the loose cartilage is removed and small holes are made in the exposed underlying bone to allow a blood clot to form which usually heals the hole in the articular cartilage with scar tissue known as 'fibrocartilage'. This procedure is known as 'microfracture'. Fibrocartilage is obviously not as good as articular cartilage, but the ankle is quite forgiving of articular cartilage damage, so this may be good enough. If the damage is very severe, your doctor will discuss cartilage cell (chondrocyte) implantation with you - this requires two operations - an arthroscopy to harvest some cartilage cells, which are then grown in the laboratory, and a second operation to glue the new cells in the ankle joint.
Instability
This diagnosis may not be confirmed until the arthroscopy. If confirmed your doctor will make a cut at the outside of the ankle and explore the ankle ligaments. If they are repairable, they will be repaired then, if they are beyond repair, they will be reconstructed.
Ligament repair
If the ligaments are loose but repairable they are stitched up tighter. This has the advantage of keeping one's own ligaments, but the disadvantage of needing to be protected in a cast for 4-6 weeks. The cast used is fibreglass with a Goretex liner (Gore Procel) and is fully waterproof, so one can swim and shower normally, and because it stays clean, it stays comfortable. After the cast is removed one needs to work hard in physiotherapy to get one's strength back.
Ligament reconstruction
If the ligaments are beyond repair, your doctor will take a hamstring tendon by a small cut just below the knee (it is not painful, and it re-grows) and use it to reconstruct the ligaments. This has the disadvantage of needing a hamstring tendon and being a bigger operation, but the advantage of providing a strong and near-anatomical reconstruction that does not need a cast. Normally one wears an AirCast Walker (www.aircast.com) just for getting about, and removes it for sleeping and bathing, until the ankle is strong enough to walk in normal shoes. This is usually 3-4 weeks.
What about rehabilitation?
Rehabilitation is crucial to recovery from ankle injuries and surgery. It is vital to follow a physiotherapy-supervised rehabilitation programme designed to regain strength and balance.
When can I return to sport?
One can return to sport when one has sufficient strength, balance, reactions, and endurance to play meaningfully and not get injured. This depends on the individual, the problem, the operation, the rehabilitation, and the sport, but usually one is ready to start training about 3 months after an ankle operation.
What are the risks?
There are general risks of any kind of surgery, including anaesthetic problems, infection and clotting (DVT or deep venous thrombosis), and these risks, and how they are minimised, are explained in the document "Information for patients having surgery at Matilda International Hospital Hong Kong with Asia Medical Specialists".
There are some risks specific to ankle arthroscopy and ligament reconstruction:
Pain - very occasionally one can have develop pain after an injury or operation because of overreaction of the nerves - this is known as 'causalgia' or 'complex regional pain syndrome'. More commonly, one may be left with some of the pain one began with despite the treatment.
Nerve damage - it is common to get a little numbness or pins & needles near or beyond any incisions, because small branches of the nerves to the skin get stretched or cut. Very rarely the bigger nerves to the foot can be injured - if so it could require a second operation to repair them, and the nerve may not fully recover.
Tendon damage - very occasionally tendons can be injured - if so it could require a second operation to repair them - usually the result would be good.
Overtightening of the ligaments - this does not really occur with the 'anatomic' operations used by Asia Medical Specialists, but, because the healed or reconstructed ligaments do not contain as much of the protein elastin as the normal ligaments, the ankle may feel stiff or tight - this is not a major problem.
References
1. Griffith, J.F. and J. Brockwell, Diagnosis and imaging of ankle instability. Foot Ankle Clin, 2006. 11(3): p. 475-96.
2. Lamb, S.E., et al., Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet, 2009. 373(9663): p. 575-81.
3. Hertel, J., Immobilisation for acute severe ankle sprain. Lancet, 2009. 373(9663): p. 524-6.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |
 Fig. 6 MRI of the ankle. The arrow shows a normal medial ligament.
Fig. 6 MRI of the ankle. The arrow shows a normal medial ligament.