Achilles Tendinopathy FAQs
Achilles Tendinopathy FAQs
written by Dr SW KONG
(Last updatd on: 15th Oct 2020)
What is Achilles tendinopathy?
The term Achilles tendinopathy is the now commonly agreed term for diseases of the Achilles tendon (Fig. 1). In the past, we used the term tendinitis, which implies the problem is inflammation. In fact, it is not an inflammatory but a degenerative problem [1]. Tendinopathy may be a final manifestation of a wide range of disease processes. There is so far no well-accepted evidence of the exact pathology and, therefore, the management strategy.
These FAQs refer to non-insertional Achilles tendinopathy.
 Fig. 1 Anatomy of achilles tendon and the related foot |
Who gets Achilles tendinopathy?
Achilles tendon problems are very common among athletes as well as the general public. They can present with pain or swelling causing functional disability. Sometimes Achilles problems cause other foot and ankle complaints eg. Painful swelling or even sudden rupture.
There are documented intrinsic and extrinsic factors that are possibly related to the problem but the association cannot easily be proven.
Intrinsic factors include aging; male gender; systemic illness; poor blood supply; lower extremity malalignment; and leg length discrepancy.
Extrinsic factors include: overuse (tendon subjected to repetitive greater-than-physiologic stresses); training errors; local or systemic steroid use; and fluoroquinolone antibiotics [2]. Achilles Tendinopathy possibly is a consequence from the combination of intrinsic and extrinsic factors [2]. Occasionally, people have swellings in their Achilles Tendon unrelated to tendinopathy, for example, those with Familial Hypercholesterolaemia get collections of cholesterol.
How is Achilles tendinopathy diagnosed?
Presentation: Patients typically complain of activity-related pain and sometimes have exquisite tenderness with or without associated fusiform swelling. The diagnosis is mostly clinical, but MRI (Fig. 2) can help to delineate more accurately extent and severity disease process or tear. Ultrasound provides an inexpensive alternative to assess the intra-tendinous pathological process [3-5]. It has been employed mostly as a real-time guide for injections of various agents.
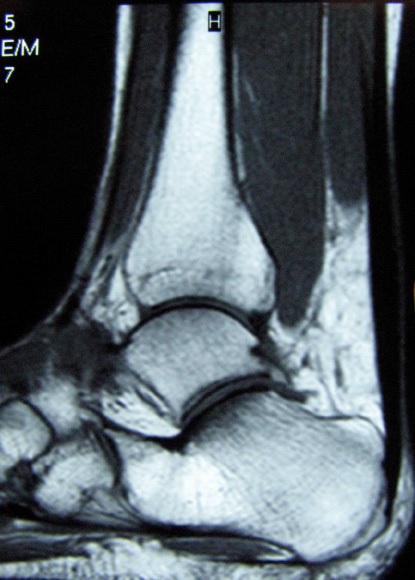 Fig. 2 MRI showing Achilles tendinopathy. |
Some patients, however, seldom have any symptom until an acute-on-chronic rupture (Fig. 3) aggregated by the sudden non-physiological action. Most patients with Achilles tendon complaints have relatively tight gastro-soleus complexes.
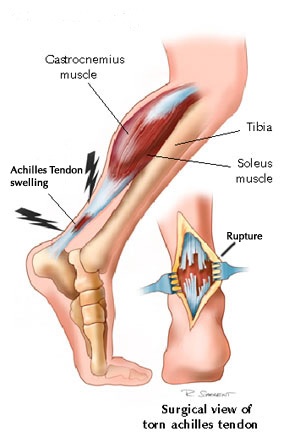 Fig. 3 Ruptured achilles tendon |
Does Achilles tendinopathy cause Achilles tendon rupture?
Not usually. Although we believe that the underlying cause of Achilles tendon rupture is tendinopathy, it is usually 'sub-clinical' ie painless so the patient is unaware of the problem. Once a patient has developed the typical pain and swelling of 'clinical' Achilles tendinopathy, it is very unusual for the tendon to rupture.
How is Achilles tendinopathy treated?
There is no consensus in treatment strategies due to the poor understanding of the disease aetiology, pathophysiology and natural history.
Most of the treatment reports are limited to case series with limited evidence bases. Generally, chronic Achilles tendinopathy responds less favorably to conservative treatment which echoes the histological evidence of a degenerative disease process that has poor capacity for healing [6].
The current literature on conservatively treated Achilles tendinopathy is largely retrospective, unsubstantiated, and lacking evidence. Nonetheless, non-operative treatment is routinely recommended, irrespective of the extent and stage of Achilles tendinopathy.
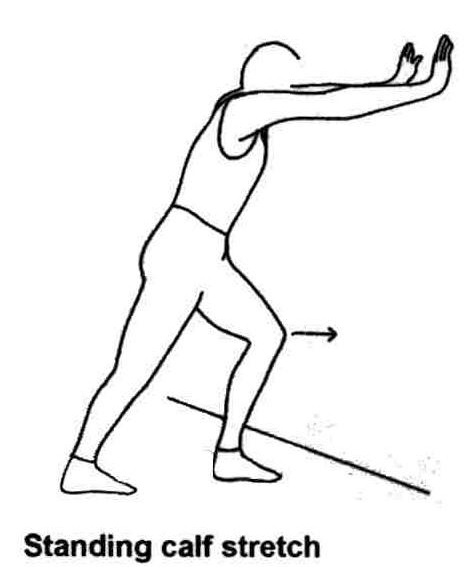
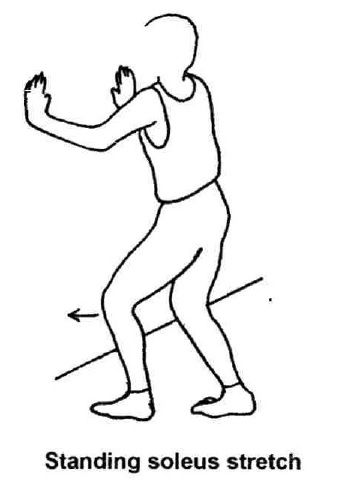
Non-operative treatment strategies, include activity modification, shoe modifications (heel lifts and orthotics), and physiotherapy, especially eccentric exercises, to stress the tendon and the gastrosoleus to improve endurance and elasticity.
Non-steroidal anti-inflammatory agents (NSAIDs), extracorporal shockwave therapy (ESWT), and topical glyceryl trinitrate have been reported to alleviate the acute painful stage with a positive effect of stimulation of the healing process.
Although NSAIDs may offer symptomatic relief in acute disease, there is no evidence that they contribute to the resolution of tendinopathy. In fact, recent literature suggests that NSAIDs may impair tendon healing [7].
Intra-tendinous injections of a sclerosing agent or corticosteroid, have been reported to be helpful in relieving symptoms, but only in small cohorts of patients [8-10].
Platelet-Rich Plasma: Injection of patient's own platelet rich plasma is a promising treatment. The principle is that the concentrated platelets provide growth factors to promote the tendon healing. It is a safe treatment with no reported side effects, as it uses only the patient's own blood.
Animal studies shows histological evidence of tendon healing and also improved quality of the healed tendon [11,12].
There are also many coming publication documenting the good response for tendon injuries, including tendon Achilles, patella tendon, hamstring, shoulder bicep tendon, tennis & golf elbow, and even acute ligament injury in ankle sprain [13].
The procedure is done in the office. 10 mls blood is drawn into a sterile syringe, and centrifuged for 5 minutes. The isolated blood serum (Fig. 4), which contains a 10-fold increase in platelet concentrate (Fig. 5), is injected directly around the diseased tendon freehand or with ultrasound guidance.
|
Rehabilitation consists of relative rest for 2-4 weeks for the tissue to heal.
The expected clinical response is improvement in pain.
Repeated injection may sometimes be required but most of the reports require only one injection.
The reported clinical experience is so far very promising though there is no high level evidence (i.e. no prospective randomised controlled trials) nor, unsurprisingly, human histology.
Eccentric calf strengthening & stretching exercises: Reports of eccentric strengthening (Fig. 6), including prospective, randomised studies, have demonstrated satisfactory results in a majority of patients [14-18], with ultrasonographic and MRI evidence of decreased tendon thickness and return to a more physiologic tendon appearance [19,20]. However, the results of eccentric strengthening may be better in athletic rather than non-athletic patients [21], and more research is needed to confirm its efficacy. Concentric loading / strengthening was believed to aggravate the already compromised tendon.
|
Surgical treatment: Recent literatures show a tendency for a more aggressive approach using surgical treatment for those who failed conservative treatment [22-26]. Factors such as increased patient age, prolonged duration of symptoms, and presence of intra-substance Achilles tendinopathy are indications for surgery.
Surgical options should be tailored to the pathological abnormality, though there is no commonly agreed treatment recommendation.
Severe disease with evidence of tendon attrition should be treated with formal open debridement of the tendon and augmentation with or without an autograft [27,28]. Moderate to mild disease is commonly treated with simple open debridement [23,29], or less invasively, with percutaneous longitudinal tenotomy [25,30] or endoscopic debridement [31].
Recently treatment with lengthening procedures, either V-Y plasty or Z-plasty or gastrocnemius recession has been advocated when there is a gastrosoleus contracture restricting ankle dorsiflexion [32,33].
References
1. Maffulli N; Kader D. Tendinopathy of tendo achilles Journal of Bone & Joint Surgery - British Volume 2002;84-1:1-8.
2. Kannus P. Etiology and pathophysiology of chronic tendon disorders in sports. Scandinavian Journal of Medicine & Science in Sports 1997;7-2:78-85.
3. Archambault JM, Wiley JP, Bray RC, Verhoef M, Wiseman DA, Elliott PD. Can sonography predict the outcome in patients with achillodynia? Journal of Clinical Ultrasound 1998;26-7:335-9.
4. Leung JL, Griffith JF. Sonography of chronic Achilles tendinopathy: a case-control study. Journal of Clinical Ultrasound 2008;36-1:27-32.
5. Peers KH, Brys PP, Lysens RJ, Peers KHE, Brys PPM, Lysens RJJ. Correlation between power Doppler ultrasonography and clinical severity in Achilles tendinopathy. International Orthopaedics 2003;27-3:180-3.
6. Vora AM, MS; Oliva, F; Maffulli, N. Tendinopathy of the main body of the Achilles Tendon Foot & Ankle Clinics 2005;10-2:293-308.
7. Li ZY, G; Khan, M; et al. Inflammatory response of human tendon fibroblasts to cyclic mechanical stretching. American Journal of Sports Medicine 2004;32-2:435-40.
8. Alfredson H, 2004. Preliminary results of colour Doppler-guided intratendi-nous glucocorticoid injection for Achilles tendonitis in five patients. Scand J Med Sci Sports 2004;14-4:269-70; author reply 70.
9. Koenig MJT-P, S; Qvistgaard, E; Terslev, L; Bliddal, H. Preliminary results of colour Doppler-guided intratendinous glucocorticoid injection for Achilles tendonitis in five patients. . Scand J Med Sci Sports 2004;14-2:100-6.
10. Alfredson HO, L. Increased intratendinous vascularity in the early period after sclerosing injection treatment in Achilles tendinosis: a healing response. Knee Surg Sports Traumatol Arthroscopy 2006;14-4:399-401.
11. de Mos M, van der Windt AE, Jahr H, van Schie HT, Weinans H, Verhaar JA, van Osch GJ. Can platelet-rich plasma enhance tendon repair? A cell culture study. American Journal of Sports Medicine 2008;36-6:1171-8.
12. Lyras DN, Kazakos K, Verettas D, Polychronidis A, Tryfonidis M, Botaitis S, Agrogiannis G, Simopoulos C, Kokka A, Patsouris E. The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot & Ankle International 2009;30- 11:1101-6.
13. Hall MP, Band PA, Meislin RJ, Jazrawi LM, Cardone DA. Platelet-rich plasma: current concepts and application in sports medicine. Journal of the American Academy of Orthopaedic Surgeons 2009;17-10:602-8.
14. Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. British Journal of Sports Medicine 2007;41-6:e3.
15. Knobloch K. Eccentric training in Achilles tendinopathy: is it harmful to tendon microcirculation? British Journal of Sports Medicine 2007;41-6:e2; discussion e.
16. Knobloch K, Kraemer R, Jagodzinski M, Zeichen J, Meller R, Vogt PM. Eccentric training decreases paratendon capillary blood flow and preserves paratendon oxygen saturation in chronic achilles tendinopathy. Journal of Orthopaedic & Sports Physical Therapy 2007;37-5:269-76.
17. Petersen W, Welp R, Rosenbaum D. Chronic Achilles tendinopathy: a prospective randomized study comparing the therapeutic effect of eccentric training, the AirHeel brace, and a combination of both. American Journal of Sports Medicine 2007;35-10:1659-67.
18. Woodley BN-W, R. J; Baxter, GD. Chronic Tendinopathy : effectiveness of eccentric exercise British Journal of Sports Medicine 2006.
19. Shalabi A. Magnetic resonance imaging in chronic Achilles tendinopathy. Acta Radiol Suppl (Stockholm) 2004-432:1-45.
20. Ohberg LA. 12(5): 465 – 70, 2004. . Effects on neovascularisation behind the good results with eccentric training in chronic midportion Achilles tendinosis. Knee Surg Sports Traumatol Arthroscopy 2004;12-5:465-70.
21. Sayana MM, N. Eccentric calfs muscle training in non-athletic patients with Achilles tendinopathy. Journal of Science Medicine Sport 2006.
22. Green DR, Ruch JA, McGlamry ED. Correction of equinus-related forefoot deformities: a case report. Journal of the American Podiatry Association 1976;66-10:768-80.
23. Scott AT, Le IL, Easley ME. Surgical strategies: noninsertional Achilles tendinopathy. Foot & Ankle International 2008;29-7:759-71.
24. Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy. A critical review. American Journal of Sports Medicine 2001;29-3:315-20.
25. Testa V, Capasso G, Benazzo F, Maffulli N. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Medicine & Science in Sports & Exercise 2002;34-4:573-80.
26. Aaron T. Scott; Ian L. D. Le MEE. Surgical Strategies: Noninsertional Achilles Tendinopathy. Foot & Ankle International 2008;20-6:759-71.
27. Coull RF, R; Stephens, MM. Flexor hallucis longus tendon transfer: evaluation of postoperative morbidity. Foot & Ankle International 2003;24-12:931-4.
28. Wilcox DB, DR; Anderson, JG. Treatment of chronic achilles tendon disorders with flexor hallucis longus tendon transfer/augmentation. Foot & Ankle International 2000;21-12:1004-10.
29. Maffulli NB, PM; Moore, D; King, JB. Surgical decompression of chronic central core lesions of the Achilles tendon. American Journal of Sports Medicine 1999;27-6:747-52.
30. Maffulli N, Testa V, Capasso G, Bifulco G, Binfield PM. Results of percutaneous longitudinal tenotomy for Achilles tendinopathy in middle- and long-distance runners. American Journal of Sports Medicine 1997;25-6:835-40.
31. Maquirriain J, Ayerza M, Costa-Paz M, Muscolo D. Endoscopic surgery in chronic achilles tendinopathies: A preliminary report. Arthroscopy 2002;18-3:298-303.
32. Costa ML, Donell ST, Tucker K. The long-term outcome of tendon lengthening for chronic Achilles tendon pain. Foot & Ankle International 2006;27-9:672-6.
33. Gentchos CE, Bohay DR, Anderson JG. Gastrocnemius recession as treatment for refractory achilles tendinopathy: a case report. Foot & Ankle International 2008;29-6:620-3.
34. Laborde JM. Neuropathic plantar forefoot ulcers treated with tendon lengthenings. Foot & Ankle International 2008;29-4:378-84.
35. Maluf KS, Mueller MJ, Strube MJ, Engsberg JR, Johnson JE. Tendon Achilles lengthening for the treatment of neuropathic ulcers causes a temporary reduction in forefoot pressure associated with changes in plantar flexor power rather than ankle motion during gait. Journal of Biomechanics 2004; 37-6:897-906.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |