Clavicle Fracture FAQs
This article has been reviewed/written by doctors of Asia Medical Specialists
(Last updated on: September 15th 2020)
Clavicle Fracture FAQs
Fractures of the collar bone (clavicle) are common and seen in all age groups.
Mechanism of injury
Most (87%) are due to a fall onto the shoulder, 7% are due to direct blow to point of the shoulder and only 6% are due to a fall onto the outstretched hand [1].
Classification
Clavicle fractures are divided into medial, mid-shaft and lateral fractures. Medial fractures are near the throat, mid-shaft are in the middle, and lateral are near the shoulder. Mid-shaft is the most common and will be discussed first, lateral are next most common, and are discussed second, and medial fractures are quite unusual and are not described in detail.
Mid-shaft Clavicle Fractures
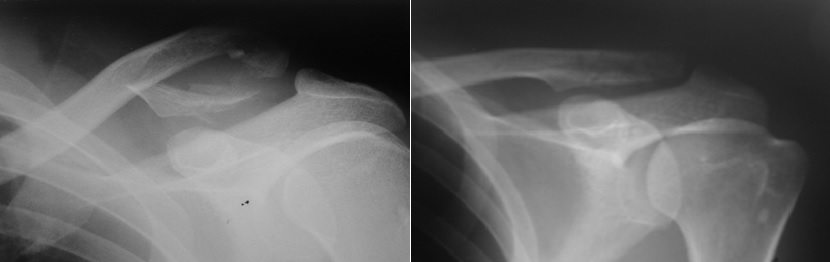
These are the most common (80%). Non-operative treatment has traditionally been the norm with the use of a simple sling for comfort for a few weeks, followed by gentle mobilisation exercises. Heavy lifting or strenuous activities should be avoided until the fracture heals, which normally takes 6 to 8 weeks. The fractures are usually quite painful for 2 weeks, and then uncomfortable for about one month. Most mild or moderate mid-shaft fractures heal without significant problems. The overall nonunion (failure to heal) rate in this type of fracture is about 2% [2].
Severe mid-shaft clavicle fractures are best treated by operation
Although non-operative treatment is the mainstay of treatment, operative treatment is indicated for severely displaced, comminuted (‘shattered’) fractures, especially if associated with high-energy trauma – for instance a fall from a height or a motor vehicle accident. Non-operative treatment of these more severe fractures has higher chance of clinically, radiologically, and subjectively unsatisfactory results due to non-union, shoulder shortening and impaired function. The chance of non-union ranges from about 8%, mostly in high energy trauma, 3% to 15% in completely displaced fractures [4]. The degree of fracture fragment displacement is the most important risk factor for nonunion [5]. Half of the patients with fracture displacement over 15mm had persistent pain with exercise [2]. A study showed that initial shortening at the fracture of more than 20 mm had a highly significant association with non-union and the chance of an unsatisfactory result [4]. The secondary neurovascular problems that may accompany a clavicular non-union include thoracic outlet syndrome, subclavian artery or vein compression or thrombosis, and brachial plexus palsy (damage to the nerves to the arm).
Reasons why one would operate on a less-severe mid-shaft fracture
1. Both sides broken – fixing one or both allows patients to look after themselves.
2. Occupational requirement - light manual workers eg surgeons, dentists and some professional sports people.
3. Injury to the nerves or blood vessels.
4. Skin ‘tenting’ and skin damage.
5. Patients with multiple injuries, even if the clavicle fracture is not too severe.
6. Relative indication is control of pain: the pain goes away much more rapidly with fixation of the broken bone.
7. Relative indication is cosmetic: There is usually an immediate deformity from the fracture, followed by formation of a large lump of healing bone (callus) (Fig. 1). Treatment with an intramedullary nail with small incision usually gives better cosmetic result.
8. Relative indication is higher risk of non-union especially in refractures.
 Fig. 1 Deformity after healing of displaced fracture clavicle |
Operative treatment
The choice of operative treatment is between intramedullary nail or plate and screws.
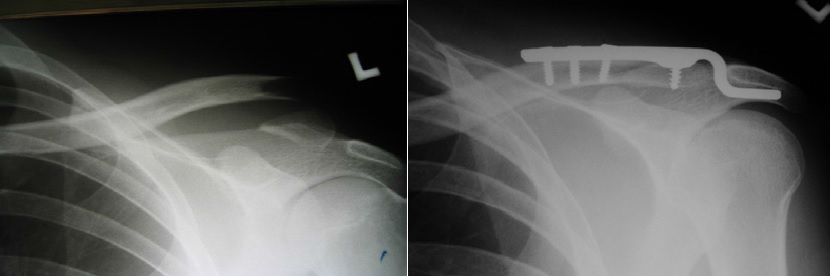
Plate and screws
Open reduction and internal fixation using plate and screws have been the standard operative treatment for mid-shaft clavicle fracture with good results.
It requires an incision along the collar bone for fracture reduction and plate application (Fig. 2). As the clavicle is frequently an exposed part of the body, especially in ladies, the scar is hard to hide.
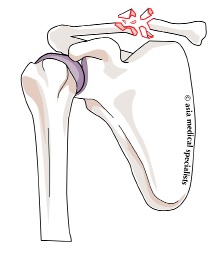 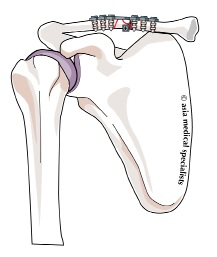 Fig. 2 Plate and screws fixation of fracture clavicle |
The plate may become quite prominent as the swelling settles, as it sits on top of the clavicle and it is only covered with skin. Sometimes there may be an area of disturbed sensation in the surrounding skin. The plate does not need to be removed routinely, but it may be removed after 6 months to 1 year when the fracture has fully healed if it is prominent or uncomfortable – this is a minor procedure.
Intramedullary Nail
As the clavicle is a tubular bone and lying in just below the skin, it is possible to pass a metal rod inside the bone via a very small cut in the skin. This technique, though attractive in theory, caused many problems of nail breakage and pin migration as the implants used were either too rigid and migrated or too thin and broke.
The new Titanium Elastic Nail (TEN) (Fig. 3) was invented primarily for treatment of humeral, femoral and tibial fractures in adolescents and children, or small statured adults. Recent studies found it is also useful for fixing displaced mid-clavicle fractures [6]. It allows for early motion and function, immediate pain reduction and the clavicle has a lower rate of fracture non-union and malunion compared to nonoperative treatment. Some studies recommend intramedullary nailing as the preferred treatment for athletes [7].
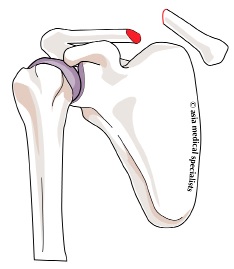 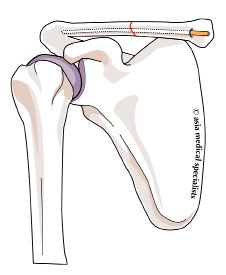 Fig. 3 Titanium Elastic Nail for Fracture Clavicle |
A small skin incision is made just above the medial end of the clavicle. A titanium nail about 3 mm in diameter is pushed inside the bone across the fracture (Fig. 4). If it is not possible to guide the nail across the fracture, a small skin incision is made at the level of the fracture to assist passing the nail.
 Fig. 4 Fracture clavicle fixed with titanium elastic nail |
Postoperatively, a sling is worn for comfort and patients are encouraged to move the arm as tolerated and to gradually use it in daily activities when the fracture healing progresses. The nail has to be removed when the fracture heals usually in 4 to 6 months' time. The TEN is only suitable for less comminuted fractures such as the simple
transverse or with butterfly fragment. For more comminuted fractures, open reduction with plate and screws may be more suitable to control the shortening.
Notable Patients
Sixties movie star Raquel Welch (Fig. 5) lay flat on her back in bed with a pad between her shoulder blades for 3 weeks to ensure a perfect cosmetic result.
 Fig. 5 Raquel Welch* |
Sir Robert Peel (Fig. 6), British Prime Minister and founder of the Police force, fell from his horse, broke his clavicle and had the sharp end of the broken bone tear his
subclavian blood vessels – he bleeded to death.
 Fig. 6 Sir Robert Peel |
Jennifer Chang, elite equestrian (show jumper) fell off her horse, shattering her right clavicle. She had plating to restore the normal anatomy, and thus function to her shoulder. She is thoroughly pleased with the results and has returned to competitive show jumping (Fig. 7).
|
Lateral Clavicle Fractures
Lateral fractures make up one-fifth of all clavicle fractures. Almost all displaced lateral clavicle fractures should be operated, as they have a very high rate of non-union, and the non-unions are very difficult to treat. There is strong evidence for treating all lateral clavicle fractures in adults.
Medial Clavicle Fractures
These are not very common (2%). Usually they heal with a sling. One must look out for a sternoclavicular joint dislocation or fracture-dislocation, which may require operative reduction. It may be difficult to judge on a plain X-ray, so CT scan may be helpful.
References:
1. Stanley D, Trowbridge EA, Noris SH. The mechanism of clavicular fracture. J Bone Joint Surg (Br) 1988;70:461-464.
2. Eskola A, Vaininonpaa S, Myllynen P, Patiala H, Rokkanen P. Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg 1986; 105:337-338.
3. White RR, Anson PS, Kristiansen T. Adult clavicle fractures: relationship between mechanism of injury and healing. Orthop Trans 1989; 13:514-515.
4. Hill JM, McGuire MH, Crosby L. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surgery 1997; 79B(4): 537-41.
5. Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg (Am) 1987; 69:753-760.
6. Rehm K, Andermahr J, Jubel A. Intramedullary Nailing of Midclavicular Fractures with an Elastic Titanium Nail. Operat Orthop Traumatol 2004; 4:365-79.
7. Jubel A, Andemahr J, Bergmann H, Prokop A, Rehm, K, Fay M. Elastic stable intramedullary nailing of midclavicular fractures in athletes. British Journal Sports Med 2003; 37(6): 480–84. * Fig 5: Photo by Alan Light.
Articles written/edited/reviewed by Doctors of Asia Medical Specialists ©2018 Asia Medical Specialists Limited. All rights reserved. |