Sweaty Palms
Sweaty Palms
Written by the doctors of Asia Medical Specialists
(Last Update on: Oct 27th 2020)
Excessive sweating in the palms (palmar hyperhidrosis) is a common condition affecting about 1 to 4% of the population [1,2]. This condition affects both work and social life. Simple tasks such as handling paper can be a problem. Important social activities like shaking hands become embarrassing, and sufferers usually try to avoid such exchanges.
Non-surgical treatment
Unfortunately non-surgical means do not work very well. Non-surgical treatment includes:
1. Applying anhydrous solutions, such as aluminum chloride: effect only partial and temporary. Long term use might cause skin problem.
2. Anti-cholinergic drugs: decrease sweating generally, not specific to palms. Side effects common.
3. Iontophoresis: either does not work or effect partial and temporary only.
4. Botox injections: effective, but injection is very painful in the palms. Effect only lasts for 3 to 4 months and repeated injections are required [3].
Surgical treatment
The operation of thoracic sympathectomy can offer permanent dryness of the palms. However, in the past, sympathectomy has not been popular because the open approach is a relatively major procedure, and carries significant operative risks such as injury to the brachial plexus, stellate ganglion and the lung [4,5,6]. The size and risks of open surgery are high for a relatively “benign” condition. Not surprisingly, physicians were reluctant to refer their patients for surgery. Now this surgery can be performed via a minimally invasive approach with minimal risk [7,8,9].
Thoracoscopic sympathectomy or endoscopic thoracic sympathectomy employs a telescope which provides a clear view. There are usually two or three small wounds which are virtually painless (figs. 1 and 2).
 Fig. 1 Three small wounds 2mm to 3mm are used for thoracoscopic sympathectomy. |
 Fig. 2 The wounds after surgery. A small catheter is used to suck out all the air at end of the operation so that chest drain is not required. |
At thoracoscopy, the sympathetic chain can be identified clearly, and the sympathetic chain is divided or partially removed (figs. 3 and 4).
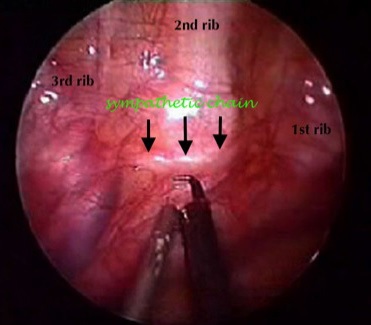 Fig. 3 View from thoracoscopy (right pleural cavity). The sympathetic chain can be clearly identified (arrowed). |
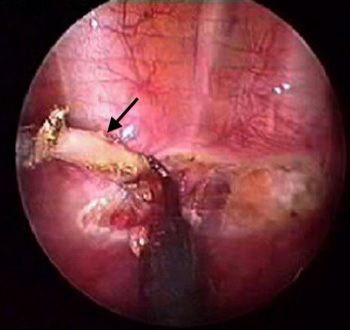 Fig. 4 The sympathetic chain (arrowed) is being dissected off the chest wall. |
Recent evidence shows that the highest success rate is achieved if sympathetic chain is divided at top of the 3rd rib [9,10]. The success rate, that is the hands become dry post-operatively, is near 100% (Fig. 5) [7,9,11].
 Fig. 5 Hands before (upper pictures) and 3 weeks after (lower pictures) sympathectomy in the same patient. The palms are completely dry after surgery. Note the hands are more red after sympathectomy due to vasodilatation. |
The most common complication is compensatory sweating (CS) which can occur in 60-70% of the patients [12]. Most cases of CS are mild and only about 5 to 10% are severe [13,14]. Limiting the extent of sympathectomy may lessens the incidence of compensatory sweating.
Because of the clear view from thoracoscopy, damage to the stellate ganglion is avoided, and therefore Horner’s Syndrome (drooping of the eyelid, pinpoint pupil and absence of sweating on the face) is rarely seen with the thoracoscopic technique [7,8]. There has not been a case of Horner’s in the author’s series of nearly 300 sympathectomies (personal data).
Other operative complications include bleeding and injury to the lung, which occur uncommonly in the experienced hands [11,14]. The operation can often be performed as day surgery [15,16,17].
Conclusion
Modern thoracoscopic sympathectomy for palmar hyperhidrosis is highly effective with nearly 100% success rate. The operative risks are low and post-operative complications are usually minor. The wounds are very small and cosmeses are excellent. It is highly recommended for persons with disturbing sweaty palms.
References
1. Haider A, Solish N. Focal hyperhidrosis: diagnosis and management. Canadian Medical Association Journal 2005;172(1):69-75.
2. Strutton DR, Kowalski J, Glaser DA, Stang P. US prevalence of hyperhidrosis: results from a national consumer panel. Poster presentation at the Annual Meeting of the American Academy of Dermatology 2003; Poster abstract P362, San Francisco, Calif.
3. Ambrosia V, Campione E, Mieo D et al. Bilateral thoracoscopic T2 to T3 sympathectomy versus botulinum injection in palmar hyperhidrosis. Ann Thorax Surg 2009 Jul;88(1):238-45.
4. Little JM, May J. A comparison of supraclavicular and axillary approaches to upper thoracic sympathectomy. Aust NZ J Surg 1975;45:143-6.
5. Kurchin A, Zweig A, Adar R, Mozes M. Upper dorsal sympathectomy for palmar primary hyperhidrosis by the supraclavicular approach. World J Surg 1977;1:667-74.
6. Adar R, Kurchin A, Zweig A, Mozes M. Palmar hyperhidrosis and its surgical treatment: a report of 100 cases. Ann Surg 1977;186:34-41.
7. Tai YP, Lee MWM, Li MKW. Thoracoscopic sympathectomy for palmar hyperhidrosis: Hong Kong early experience. HK Med J 1996;2(3):315-8.
8. Li X, Tu YR, Lin M et al. Minimizing endoscopic thoracic sympathectomy for primary palmar hyperhidrosis: guided by palmar skin temperature and laser Doppler blood flow. Ann Thorac Surg 2009 Feb;87(2):427-31.
9. Deng B, Tan QY, Jiang YG et al. Optimization of sympathectomy to treat palmar hyperhidrosis: the systemic review and metaanalysis of studies published during the past decade. Surg Endosc 2011 Jun;25(6):1893-901.
10. Cerfolio RJ, De Campos JR, Bryant AS et al. The society of thoracic surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 2011 May;91(5):1642-8.
11. Liu Y, Yang J, Liu J et al. Surgical treatment of primary hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg 2009 Mar;35(3):398-402.
12. Araujo CA, Axevedo IM, Ferreira MA et al. Compensatory sweating after thoracoscopic sympathectomy: characteristics, prevalence and influence on patient satisfaction. J Bras Pneumol 2009 Mar;35(3):213-20.
13. Li X, Tu YR, Lin M et al. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2-4 ablation. Ann Thorac Surg 2008 May;85(5):1747-51.
14. Rodriguez PM, Freixinet JL, Hussein M et al. Side effects, complications and outcome of thoracoscopic sympathectomy for palmar and axillary hyperhidrosis in 406 patients. Eur J Cardiothorac Surg 2008 Sep;34(3):514-9.
15. Cameron A. Early experience with day-case transthoracic endoscopic sympathectomy. Br J Surg 1999 Jan;86(1):139.
16. Hsia JY, Chen CY, Hsu CP et al. Outpatient thoracoscopic limited sympathectomy for hyperhidrosis palmaris. Ann Thorac Surg 1999 Jan;67(1)258-9.
17. Miller DL, Force SD. Outpatient microthoracoscopic sympathectomy for palmar hyperhidrosis. Ann Thorac Surg 2007 May;83(5):1850-3.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |
