The New Concept and the Latest Advances in Stroke Management
The New Concept and the Latest Advances in Stroke Management
written by doctors of Asia Medical Specialists
(Last update on: Oct 28th 2020)
Summary
The old concept of ‘Cerebrovascular Accident” is recently replaced by the new concept of “Brain Attack”. Just like heart attack, brain attack is also an acute cardiovascular disease. Both heart attack and brain attack are of similar etiologies. The concept of treatment for heart attack also applies to brain attack. For heart attack, cardiologist prefers Percutaneous Coronary Intervention, the cardiac-PCI rather than intravenous recombinant tissue plasminogen activator (e.g. iv rtPA). Cardiac-PCI has to be performed within 12 hours after symptom onset. IV rtPA is thus the 2nd line treatment for heart attack, offered only if PCI is not available.
Similar concept also applies to brain attack. Vascular neurosurgeon also prefers Percutaneous Cerebral Intervention (Neuro-PCI), rather than iv rtPA. The Neuro-PCI has to be performed within 8 hours after symptom onset. This is thus the new Golden-8-hours Concept for brain attack. Nowadays Neuro-PCI is the first line standard treatment offered by most Comprehensive Stroke Centres in US. Iv rtPA within Golden-3-hours is considered to be the 2nd line treatment, offered only when Neuro-PCI is not available.
|
The New Concept of Stroke
The old concept of cerebrovascular accident and the acceptance of the fate of gradual neurological deterioration and the final state of disability, or even death, should have a revolutionary change. The new term “Brain Attack” implies that stroke is not an accident. Just like a heart attack, a stroke is something preventable, treatable, or even curable, without leaving patients with any neurological deficits. Strokes can be tackled in a similar way to heart attacks. In future, patients suffering from acute ischemic strokes will be less miserable [1,2].
What is a stroke?
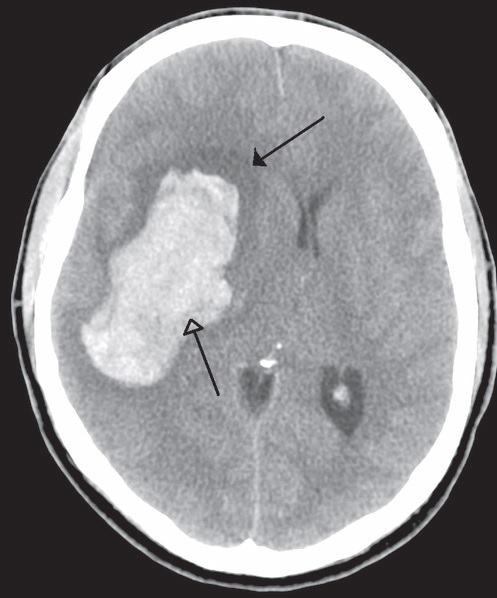
The term “stroke” refers to the sudden onset of neurological impairment due to vascular causes. There are two types of stroke: Ischaemic stroke accounts for ~87% of all strokes in the western world (~70% in Hong Kong). Haemorrhagic stroke explains the remaining 13% (~30% in Hong Kong). Yet haemorrhagic stroke has a higher mortality than the ischaemic entity; it is responsible for more than 30% of all stroke deaths.
Pathophysiology
Strokes can strike individuals regardless age, race or gender. During ischaemic stroke, a blood vessel in the brain becomes blocked. The blockage disrupts the blood flow, preventing oxygen from being delivered to the area of the brain affected. The section of brain tissue deprived of oxygen becomes “stunned” and no longer functions properly, resulting in the stroke symptoms.
Time is Brain
Acute ischaemic stroke (AIS) is a serious medical emergency. Rapid intervention is crucial. For every minute a large vessel stroke goes untreated, as many as 1.9 million neurons are lost (32,000 neurons are lost per second, 120 million neurons are lost per hour), 14 billion synapses are lost , 7.5 miles of myelinated fibers are lost. Permanent neurologic damage is more likely to occur the longer a stroke goes untreated. If treatment is delayed, additional death of critical brain cells occurs “infarction” reducing the potential benefit of the treatment. A short time to treatment is absolutely critical to increase the probability of a good recovery. After approximately three hours, brain cells will suffer irreversible injury usually leading to their death. This is the reason why thrombolytic therapy of rtPA are given only until three hours since the onset of the stroke. Therefore time really is brain [3].
Epidemiology and Socio-Economic Impact
1. Each year roughly there are 18,000 stroke cases in Hong Kong. Each year roughly 795,000 Americans experience a new (610,000) or recurrent (185,000) stroke.
2. Stroke is the third leading cause of death in the United States, behind heart disease and cancer. It has been estimated that ~60,000 Americans will die from stroke every year. It causes 10% of deaths worldwide [4].
3. The incidence of stroke is expected to rise in coming decades due to aging populations. It could soon be the most common cause of death worldwide 5.The incidence of stroke increases exponentially from 30 years of age, and aetiology varies by age [6].
4. Stroke is the leading cause of severe, long-term disability.
5. Stroke is the number one cause of inpatient Medicare reimbursement for long-term adult care. Total stroke costs now exceed $63 billion per year in the US. The estimated direct and indirect cost of stroke for 2010 is $73.7 billion.
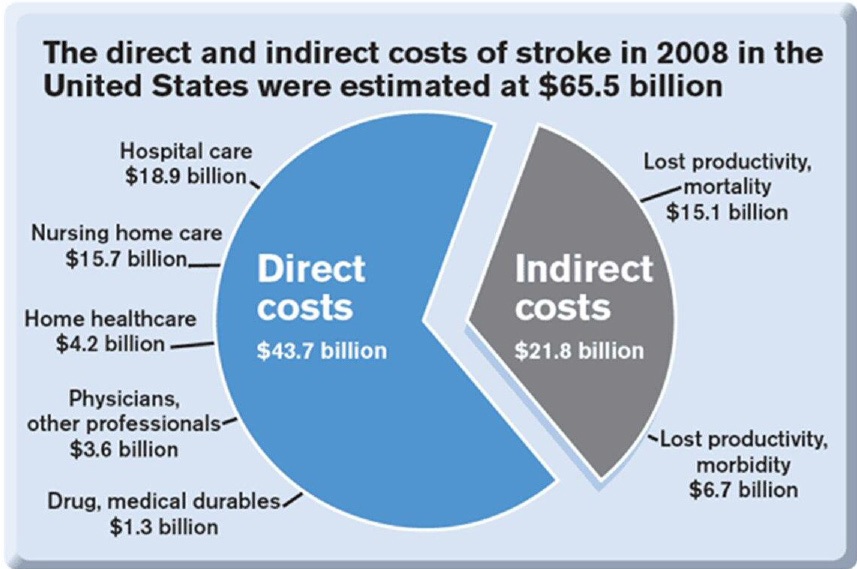 Fig. 2 Total stroke cost in US |
6. The personal and financial loss of the more than 3,000,000 people currently living with stroke is enormous.
7. Apart from physical and financial burden, stroke also exerts great psychological impact to patients and their family members.
The New Concept of Stroke Management
The new concept emphasises screening of stroke risk, the control of risk factors and the prevention on brain attack; public education on stroke symptoms allowing rapid recognition and seeking of emergency help; and, most importantly, fast-track treatment of acute brain attack during the golden hours of the therapeutic window.
QT3
Question, Screening, Prevention, Time, Place, Person, 3D8P
(QSP-TPP-3D8P)
Screening for Stroke: Question, Screening, Prevention
- Question: Ask patients questions: their own estimation of life time stroke risk (reflecting their awareness of own health and family history)
- CLIS Screening: (Clinical screen, Laboratory screen, Image screen).
a. Clinical screen:
i. SDHHH History (personal and family): Stroke, Diabetes, Hyperlipidemia, Hypertension, Heart disease.
ii. BHCBP Examination: Body Mass Index, Heart status, Carotid artery for bruit, Blood pressure, Pulse for atrial fibrillation.
b. GOCO Laboratory screen: Glucose level, (Oil) Lipid profile, Clotting profile , (Organs) Liver and Renal function.
c. Image screen: Magnetic Resonance Imaging of brain, brain vessels and carotid and vertebral arteries. - Prevention of stroke or Risk factors control: (Up to 80% of strokes are preventable; you can prevent a stroke.
a. DEWCAD Lifestyle Modification: Diet (Calorie intake, Glucose, Fat, Salt consumption) [7], Exercise, Weight, Cigarettes 8 , Alcohol 9, Drug (Oral contraceptive pills, soft drugs [10])
b. POGAS Medical Therapy: Drug for Blood pressure control11, Cholesterolaemia [11], Glucose control for diabetes [12], Atrial Fibrillation (Anticoagulant)13, Stroke in the past (Antiplatelet)
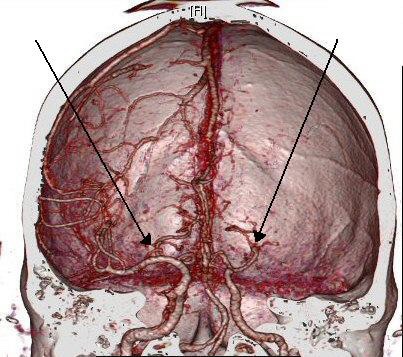
c. Structural abnormalities with or without symptoms: Refer to vascular nerosurgeon for Prophylactic Neurosurgery Percutaneous Cerebral Intervention (Neuro-PCI)
i. Cervical arteries stenosis: i.e. carotid stent for carotid stenosis [14].
ii. Intracranial vascular anomaly: e.g. hypoplastic vessels in circle of Willis: only acknowledge and aware.
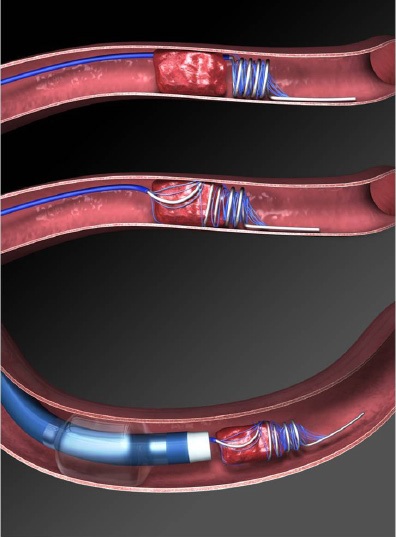
iii. Intracranial vascular stenosis: i.e. Intracranial vascular stent for Middle Cerebral Artery (MCA) stenosis [15].
iv. Cerebral aneurysm or arteriovenous malformation: Endovascular embolisation therapy for reducing the risk of haemorrhagic stroke.
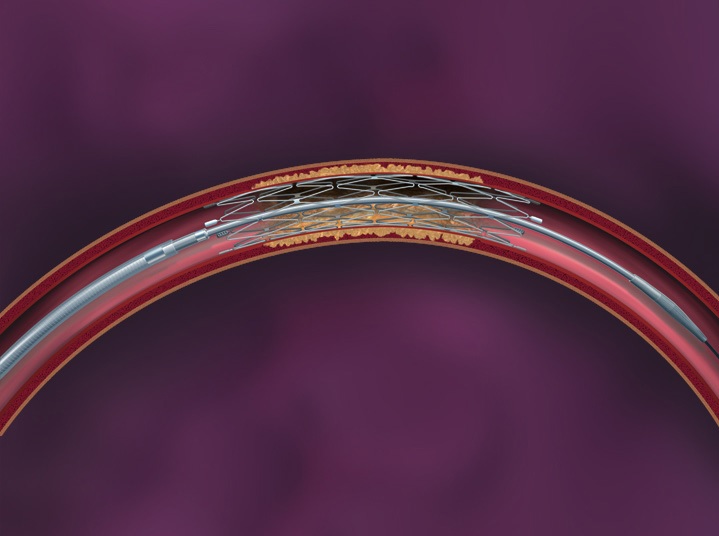 Fig. 3 The Wingspan system of intracranial vascular stent |
Management of Acute Stroke (TPP-3D8P)
Time--Place--Person--3 Golden hours Drug or PCI—8 Golden Hours only PCI (TPP-3D8P)
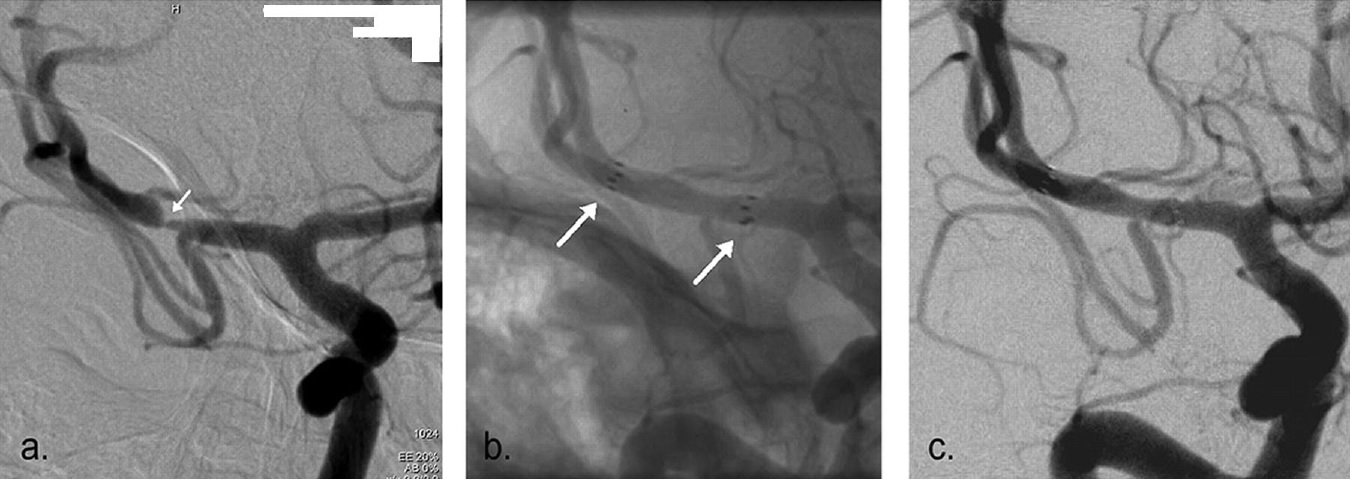 Fig. 4a The Pre-stenting angiogram (DSA) showing right MCA stenosis, b. stent-in-situ with stent marker (white arrow), c. the post-stenting DSA |
1. Time:
- Establish the exact time of symptoms onset or the time when patient was last seen to be normal. Recognition of stroke symptoms i.e. facial appearance, limbs weakness, speech problem,visual and sensory disturbance, gait and coordination, orientation and consciousness, etc.
- Promptly seek for emergency help during the Golden-3-Hours therapeutic window.
2. Place:
Seek immediate medical assessment and treatment in Hospital equipped with CT scanner, MRI scanner and Angiogram machine [16].
3. Person:
Seek help from vascular neurosurgeon who can provide comprehensive treatment and who can manage the complications associated with ischaemic stroke and its treatment.
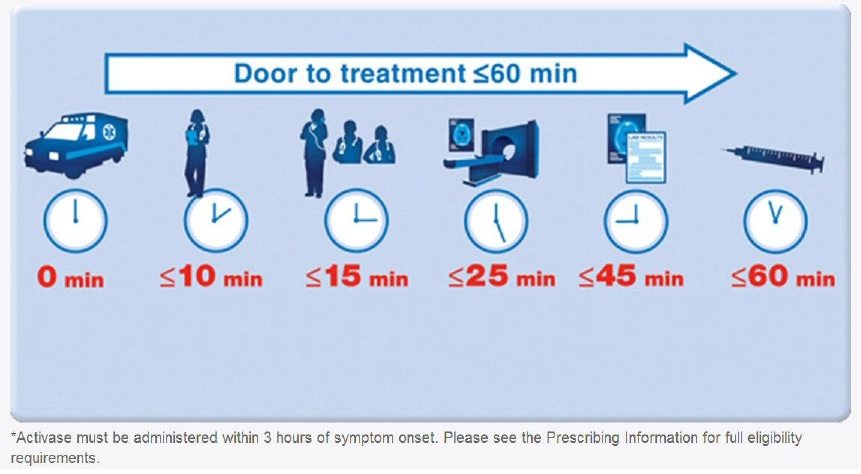
4. 3-Golden-hours Drug or PCI:
- After clinical assessment of the contraindications for intravenous recombinant tissue plasminogen activator (iv rtPA or ‘Activase’), the fibrinolytic drug may be given as the first line treatment if the option of Neuro-PCI is not available.
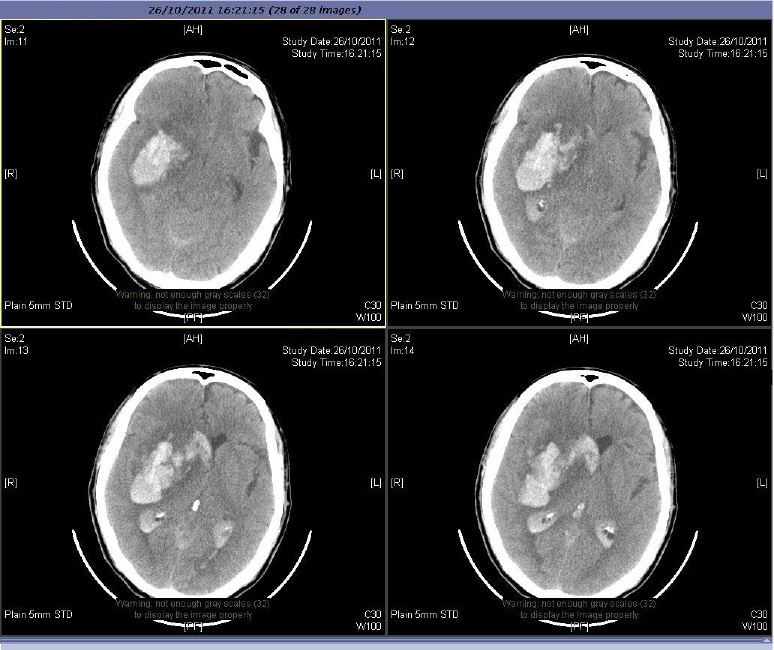
- Most (>90%) of the acute ischaemic stroke patients will not benefit from iv rtPA due to: i. late presentation to emergency room (more than 2 hours after symptom onset), ii. fall into the exclusion criteria of iv rtPA, iii. delayed diagnosis in emergency rooms or clinical wards due to misinterpretation of CT scan.
- The benefit of iv rTPA should weighted against its associated high risks. Properly informed consent is vital [17, 18].
|
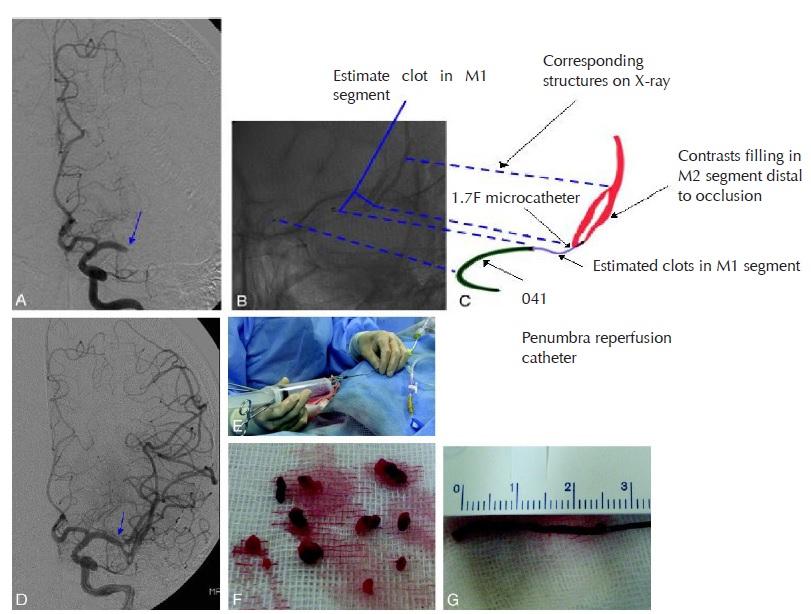
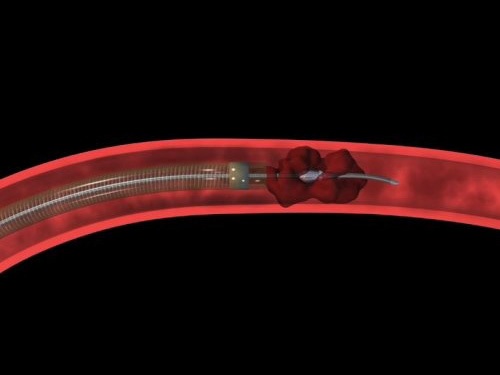
5. 8-Golden-Hours only PCI (Neurosurgical Percutaneous Cerebral Intervention)
- Neuro-PCI achieves brain revascularisation by mechanical thrombectomy under fluoroscopic guidance of cerebral angiograms. A micro-catheter is passed up to the occluding thrombus in intracranial vessels. The thrombus or embolus is removed by the device using mechanical breakage and aspiration.
- Intra-arterial fibrinolysis i.e. ia rtPA injected at the site of thrombosis, improves outcomes in acute ischemic stroke [19] .
- Intra-vascular stent may be deployed if concomitant vascular stenosis exists.
- Within the Golden-3-hours, Neuro PCI can revascularise the brain cells and minimise the central infarction core. Patients may have full recovery without any neurological deficit.
- Within the Golden-8-Hours: From the therapeutic window of the 4th hour to the 7th hour, Neuro-PCI revascularisation can salvage brain cells in the peripheral ischaemic region called the Penumbra Zone and minimise the volume of brain infarction. Thus the overall morbidity and mortality of ischaemic stroke is reduced.
- Neuro-PCI is also indicated for patients who were unable to receive iv rtPA due to contraindications or for whom the drugs were ineffective [20, 21, 22, 23].
|
Salvage Neurosurgery
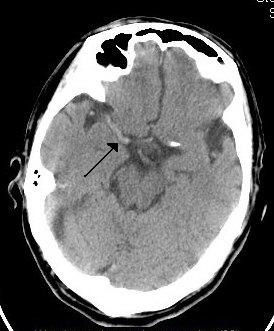
1. Surgery for bleeding complication of iv rtPA
Around 6% of iv rtPA treated patients develop symptomatic intracranial bleeding that cause more disastrous brain damage [24]. Salvage neurosurgery is difficult due to rtPA caused bleeding tendency. Though surgery may be lifesaving, patients may be severely disabled or even vegetative.
|
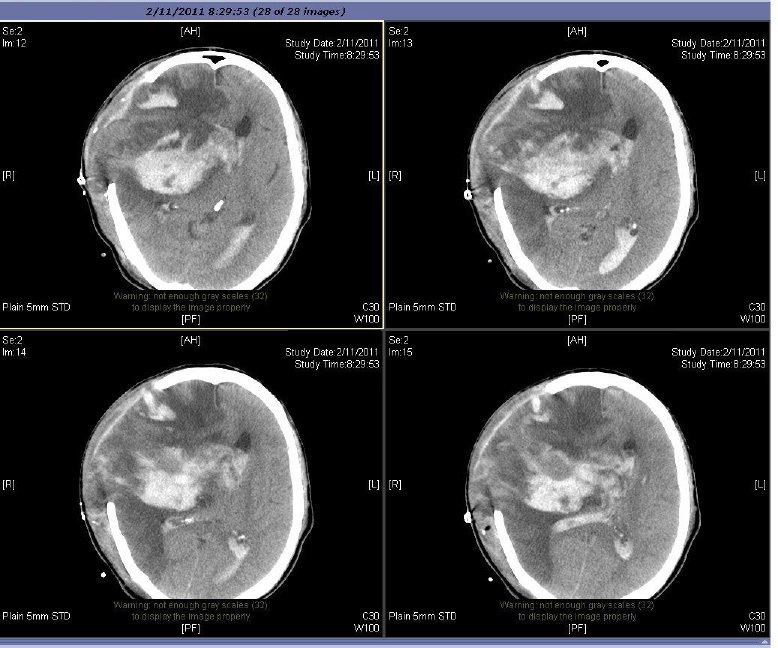
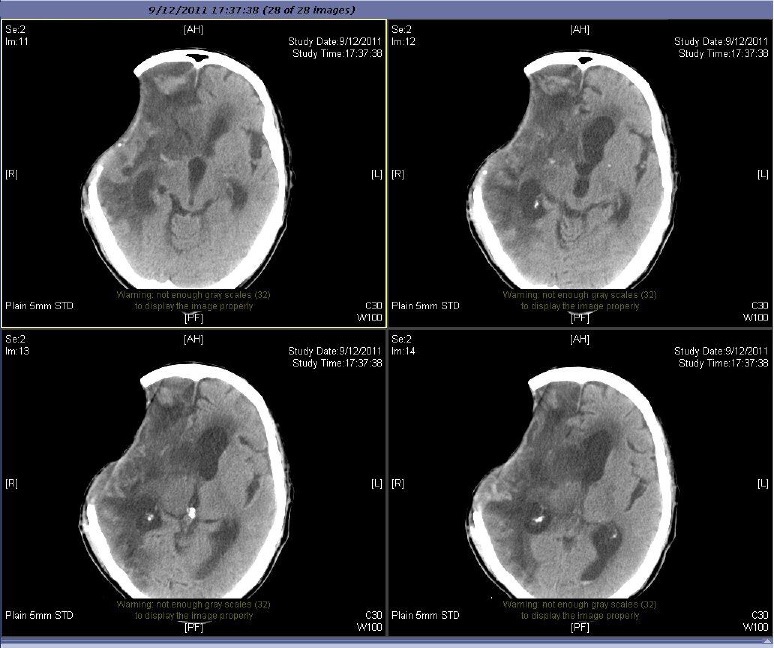
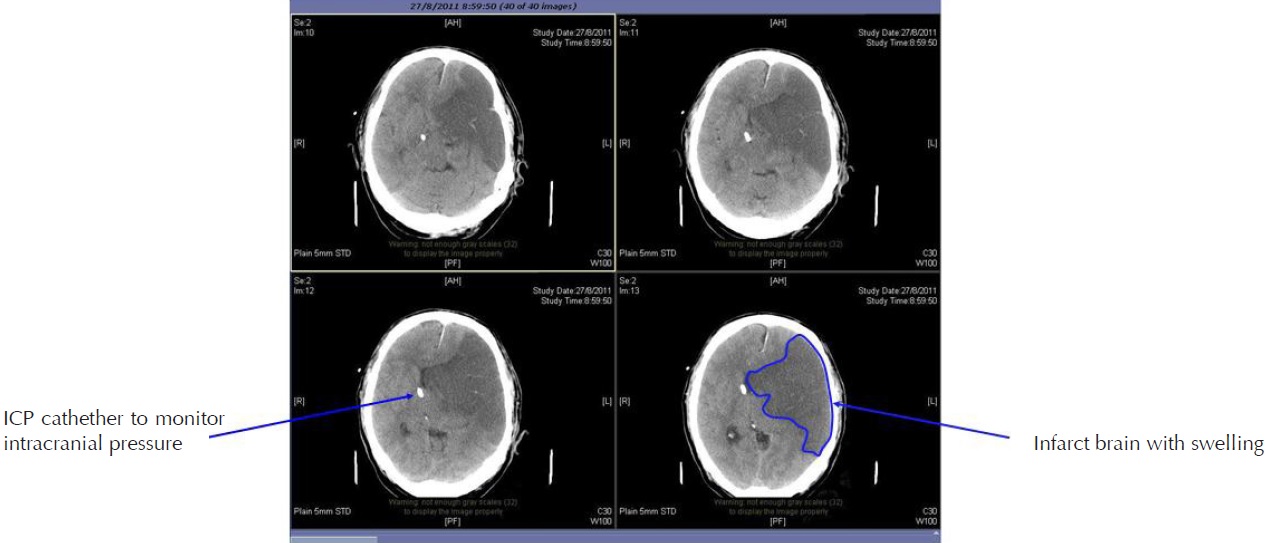
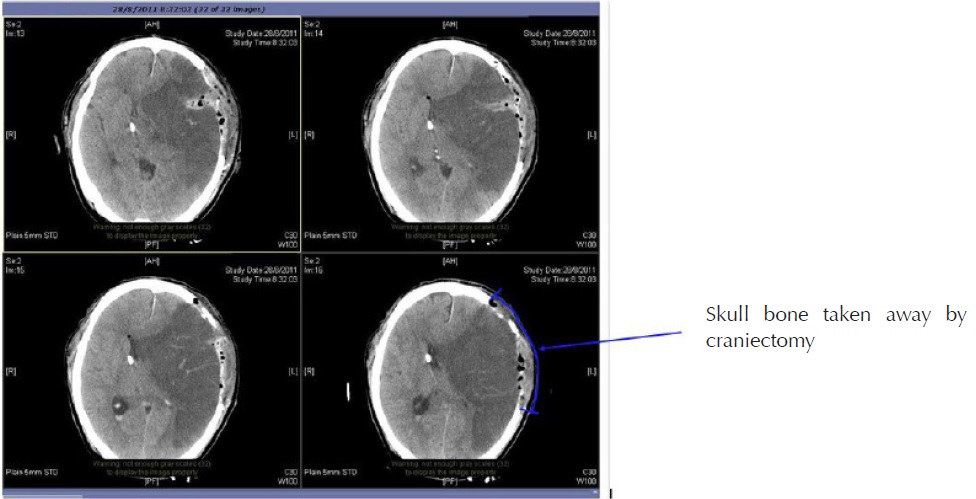
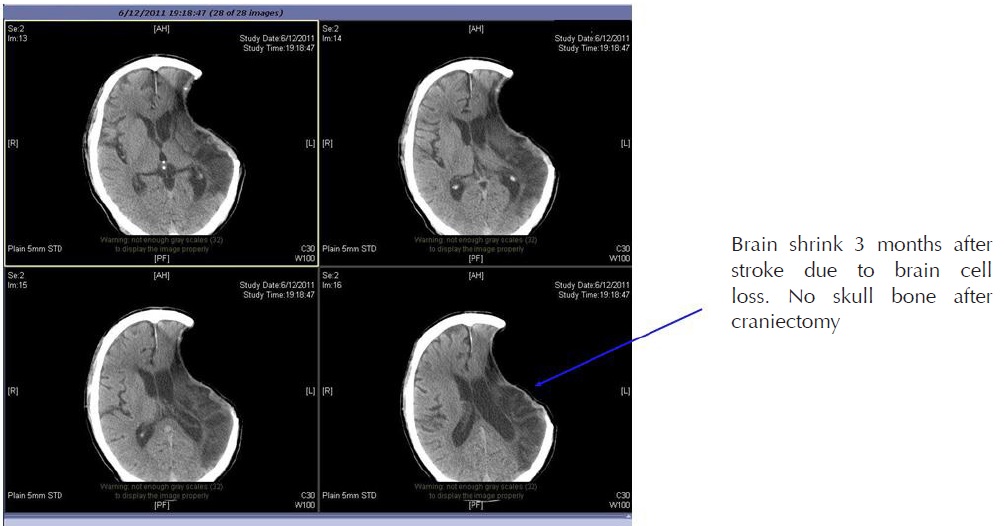
2. Cranial Decompressive Surgery: Craniectomy +/- Lobectomy
Large territory strokes can cause significant oedema of the brain with secondary brain injury in surrounding tissue. This phenomenon is mainly encountered in strokes of the middle cerebral artery territory, and is also called “malignant cerebral infaction” because it carries a dismal prognosis. Relief of the pressure may be attempted with medication, but some require decompressive craniectomy (temporary surgical removal of the skull) +/- lobectomy with excision of infarcted brain tissue. This confers a marked improvement in the risk of death, although most survivors are disabled [25].
|
References
1. World Health Organisation (1978). Cerebrovascular Disorders (Offset Publications). Geneva
2. Kidwell CS, Warach S (December 2003). “Acute ischemic cerebrovascular syndrome: diagnostic criteria”. Stroke 34 (12): 2995–8
3. Saver JL (2006). “Time is brain - quantified”. Stroke 37 (1): 263–6
4. The World health report 2004. Annex Table 2: Deaths by cause, sex and mortality stratum in WHO regions, estimates for 2002. Geneva
5. Murray CJ, Lopez AD (1997). “Mortality by cause for eight regions of the world: Global Burden of Disease Study”. Lancet 349 (9061): 1269–76.
6. Ellekjær, H; Holmen J, Indredavik B, Terent A (November 1, 1997). “Epidemiology of Stroke in Innherred, Norway, 1994 to 1996 : Incidence and 30-Day Case-Fatality Rate”. Stroke 28 (11): 2180–2184
| ©2017 Asia Medical Specialists Limited. All rights reserved. |