Patellofemoral Pain
Patellofemoral Pain
article written by Dr CC KONG
(Last updated on: Oct 13th 2020)
Anterior Knee Pain – or pain at the kneecap - is a very common complaint. Most anterior knee pain is from the joint between the kneecap (patella) and the thigh bone (femur), known as the patellofemoral joint. This article looks at the assessment and treatment options of anterior knee pain.
Patellofemoral biomechanics
The patella is a sesamoid bone in the knee extensor tendon. Its function is to reduce friction and improve leverage as the knee bends through its giant arc of motion. It is subjected massive loads, up to several times body weight, as the knee bends, and therefore has the thickest articular cartilage in the body. The patella articulates with the trochlea groove in the femur to form the patellofemoral joint. When the knee is straight the patella 'floats' without much constraint, and as the knee bends the patella enters the trochlea groove.
The patella connects the quadriceps tendon in the thigh to the patellar tendon below the knee attaching to the tibial tuberosity of the shin bone.
On the inside and outsides of the patella are the medial and lateral retinaculae – sheets of tough fibrous tissue which stop the patella from moving too far from side to side.
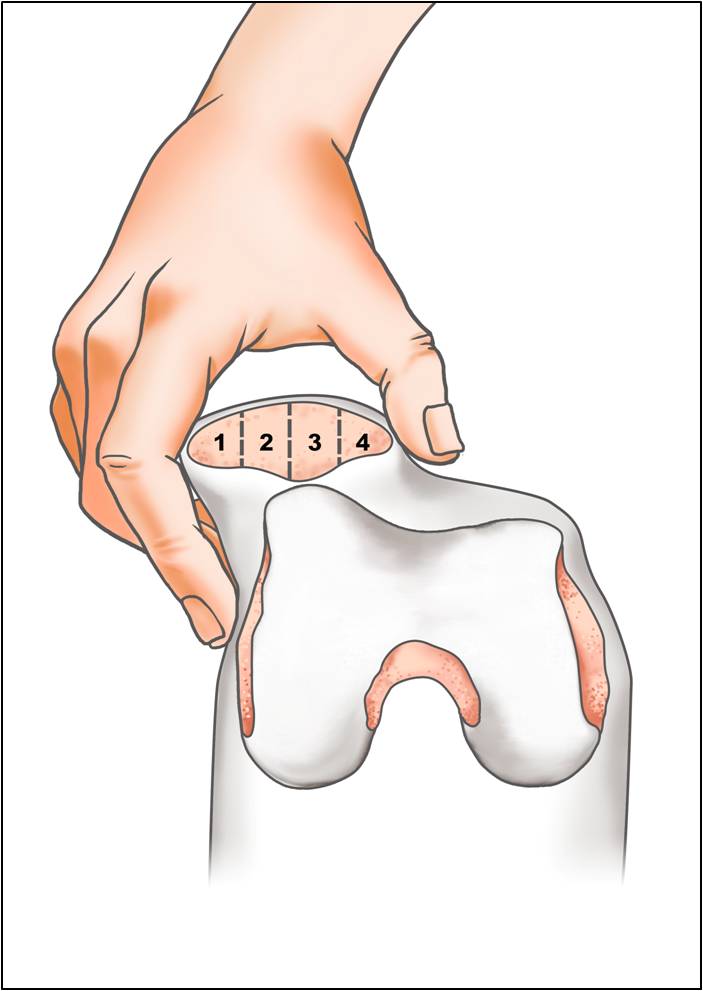
Ideally the forces acting on the patella are balanced, to provide stability and maintain proper tracking (Fig. 1).
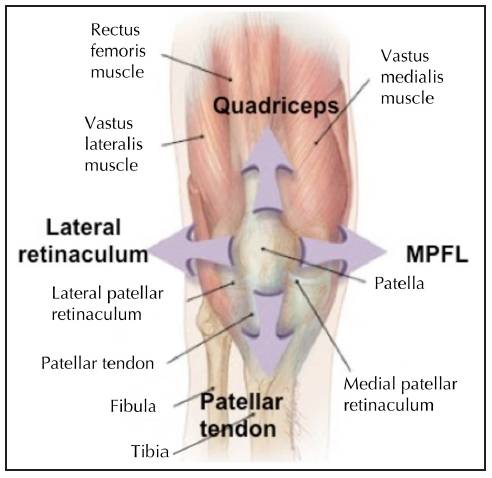 Fig.1 Forces acting on the patella |
Even minor alterations in the knee joint mechanics can profoundly affect patellofemoral loads. Flatow [1] showed a dramatic reduction of contact area with simulated 5 degrees tilting and 5mm sideways shifting of the patella, causing very high peak loads on the cartilage, which could result in pain, cartilage damage, and arthritis.
Patellofemoral Pain Assessment
Accurate diagnosis is the basis of successful treatment. The followings are the assessments that a practitioner would perform.
- History
- Examination
- Look and Feel
- Move
- Radiology
History. Patients describe pain primarily in the front of their knees, worse with stairs - especially going down. They frequently experience pain with prolonged sitting (e.g. watching a movie, or sitting in an aeroplane) and feel that they have to straighten their legs to decrease discomfort occasionally. The pain is usually exacerbated by squatting and kneeling. It is generally an aching pain but can be sharp or burning. This occurs particularly when going down the stairs. The problem often begins after taking up a new activity or increasing the intensity of an activity.
One of the most important features is giving way. The patient may report that something jumps in the knee or something is out of place momentarily, causing a sense of instability. Sometimes people fall down.
Examination. The goals are to locate the painful structure and to assess factors that affect patellar forces and alignment.
- Look
- Valgus (knock) knees
- 'Squinting' patellae (Fig. 2)
- Flat feet
- Increased foot progression angle (Charlie Chaplin)
- Decreased foot progression angle ('pigeon toed')
- Positive "J sign" (the patella following an upside down J shaped track - moving sideways on knee extension as it leaves the trochlea groove and is pulled laterally by tight lateral structures)
 Fig. 2 Squinting patellae |
- Feel
- Patellar tenderness
- Infrapatellar fat pad tenderness
- Patellar tendon tenderness
- Quadriceps tendon tenderness
- Tender pre-patellar, infra-patellar or anserine bursae
- Move
- Generalised ligament laxity, according to Beighton's criteria [2] (Table 1), which is associated with patellar instability.
- Active and passive knee motion
- Patellar crepitus
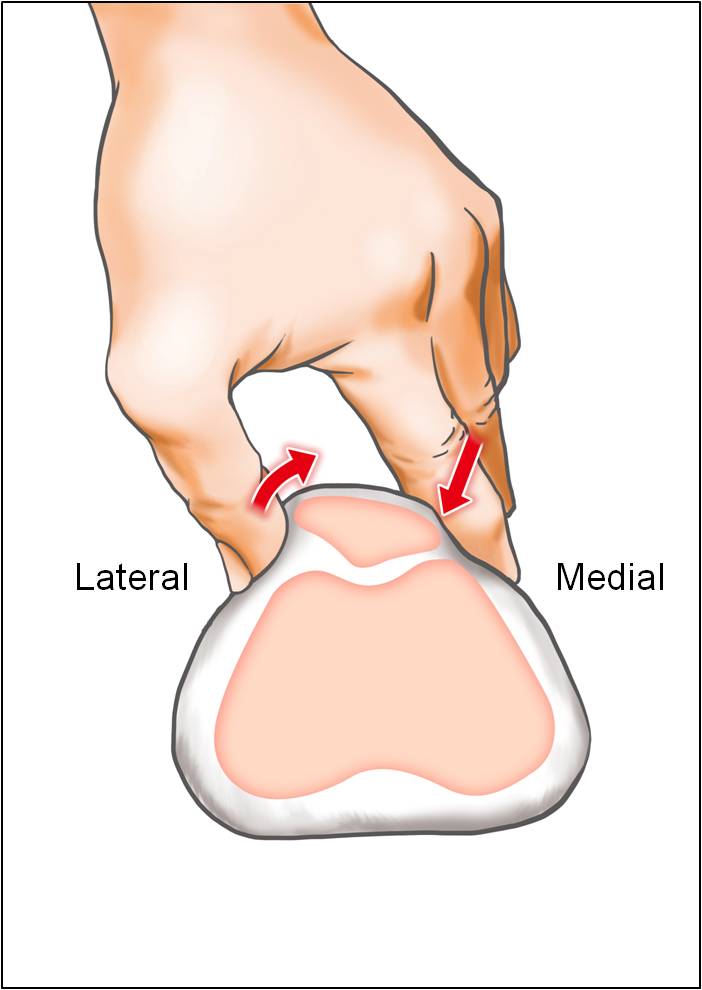
- Patellar glide test (Fig. 3)
- Patellar tilt test (Fig. 4)
- Knee ligament stability – especially PCL laxity, which increases patellofemoral pressures
- Hip rotation – internal and external rotation should be equal – if not there may be a torsional deformity
- Thigh foot angle is measured to identify torsional deformity
| Table 1 | Left | Right | |
| 1 | Passive hyperextension of the little finger MCP joint beyond 90° with the forearm and hand flat on a table | 1 | 1 |
| 2 | Passive apposition of the thumb to the flexor aspect of the forearm | 1 | 1 |
| 3 | Passive hyperextension of the elbow beyond 10° | 1 | 1 |
| 4 | Passive hyperextension of the knee beyond 10° | 1 | 1 |
| 5 | Active forward flexion of the trunk with the knees fully extended so that the palms of the hands rest flat on the floor | 1 | - |
| Total | /9 | ||
Fig. 3 Patellar gliding test. The kneecap can be manually displaced both medially and laterally between 25% and 50% of width of the patella. Minimal displacement signifies retinacular tightness. |
Radiology
- X-rays. Three views for patellofemoral problems:
- anteroposterior
- true lateral (Fig. 5)
- Laurin's skyline view (Fig. 6) with the knee in 30 degrees flexion
- Computerised tomography (CT) is used to assess the rotational alignment of the lower limb – looking for torsional deformities of femur and tibia. This requires scanning the hip, knee and ankle at the same time.
- Magnetic resonance imaging (MRI) will reliably demonstrate the knee ligament conditions and cartilage problems around the patella.
|
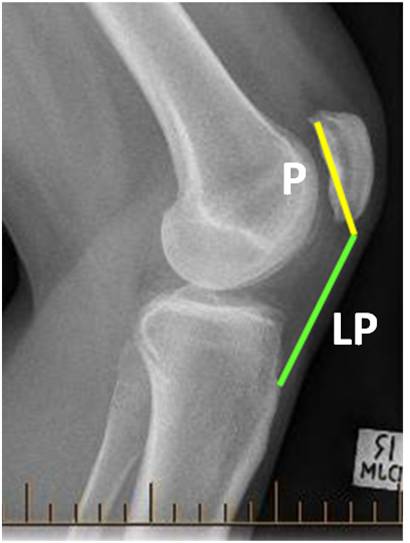 Fig. 5b 'Patella alta' with increased Insall-Salvati ratio. |
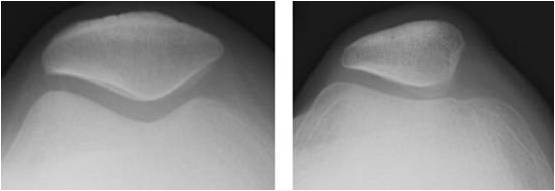 Fig. 6 Laurin's views: left: normal; right: dysplastic trochlea and patella. |
Treatment
If specific underlying damage, such as posterior cruciate ligament ruptures or meniscal tears are identified, these are treated. Bursitis (housemaid's or clergyman's knee) also has specific treatment. If no specific damage is identified, treatment is directed to the patellofemoral joint.
Biomechanical patellofemoral pain syndrome
This is pain at the front of an apparently undamaged knee, thought to be from abnormal mechanical stresses to the patellofemoral joint. The precise cause of the pain is not clear [3], however the symptoms are thought to be from the abnormalities outlined above, which cause excessive loads on the patellofemoral joint surfaces.
Treatment:
• Activity modification (avoiding activities that bring on symptoms such as climbing stairs, squatting or lunging)
• Physiotherapy supervised stretching and strengthening programme – particularly:
o Gluteus maximus stretches
o Quadriceps strengthening [4]
• Anti-inflammatory medication – for temporary pain relief – especially to allow physical therapy exercises
• Orthotics to correct flat feet, though data is slightly inconclusive
Operation:
Arthroscopy. Lateral retinacular release is suggested if non-operative treatments. It is particularly helpful in patients with tilted patellae because of lateral retinacular tightness. It may be combined with medial retinacular tightening, both of which can be performed by a minimally invasive arthroscopic procedure [5-7].
Rotational osteotomy. If the CT scan reveals that the thigh bone and/or the shin bone are twisted, causing the knee to face the wrong direction, this can be corrected by operation to twist the bones into the correct position.
The procedure involves cutting the bones ('osteotomy') and fixing them in the correct position while they heal. This can be very helpful [8, 9], including in patients who have had other knee operations, but have continuing pain [10].
Isolated patellofemoral osteoarthritis
Isolated patellofemoral arthritis occurs in about 10% of patients with knee osteoarthritis. It may be caused by injury or may follow chronic biomechanical patellofemoral pain. Patellofemoral arthritis (Fig. 7) occurs when the articular cartilage in the trochlear groove of the femur and on the underside of the patella wears out. When the wear is severe, the underlying bone may become exposed. Moving the bones along this rough surface is painful.
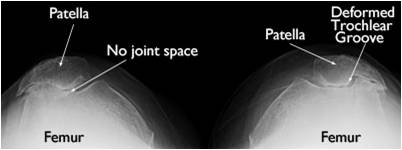 Fig. 7 Osteoarthritis of patellofemoral joint |
Initial treatment is a combination of treatment of biomechanical patellofemoral pain and of osteoarthritis in general:
• Glucosamine 1.5 grams once a day long-term [11, 12]
• Activity modification (avoiding activities that bring on symptoms such as climbing stairs, squatting or lunging)
• Physical therapy supervised stretching and strengthening programme – particularly:
o Gluteus maximus stretches
o Quadriceps strengthening [5]
• Anti-inflammatory medication – for temporary pain relief – especially to allow physical therapy exercises
• Visco-supplementation (e.g. hyaluronic acid injections)
Surgery is an option if non-operative treatment fails.
The type of surgical procedures depends on the severity of the arthritis and associated causes:
• Arthroscopy: lateral retinacular release +/- medial plication +/-chondroplasty. A minimally invasive arthroscopic procedure can help. In chondroplasty the rough arthritic joint surfaces are smoothed, which reduces catching. Chondroplasty is an option in cases of mild to moderate cartilage wear
• Tibial tuberosity transfer also called Fulkerson osteotomy (Fig. 8). This procedure can help relieve pain in patients with arthritis in specific portions of the patella. Shifting the tibial tuberosity, which is the insertion of the patellar tendon onto the shinbone, changes the position of the kneecap, reducing pressure on the arthritic areas and relieving pain [13].
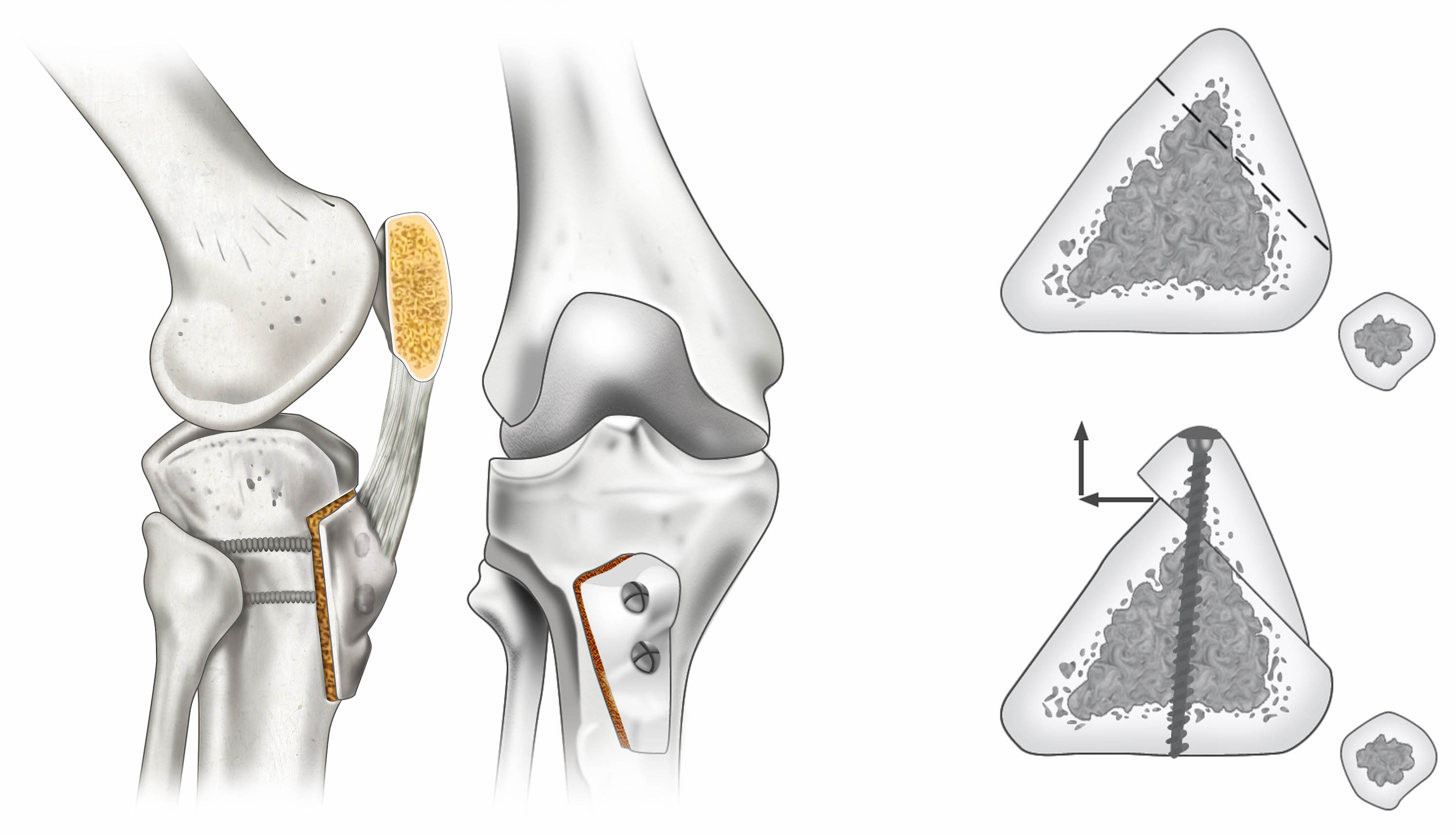 Fig. 8 Fulkerson osteotomy |
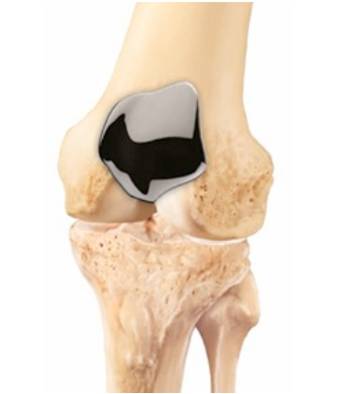
• Patellofemoral replacement. This is a partial knee replacement. The worn cartilage surfaces are removed and replaced with thin metal and plastic implants. The trochlear groove is covered by a thin metal cover (Fig. 9) and a polyethylene button is used on the patella (Fig. 10).
This is a relatively new form of knee replacement, but the medium-term results are generally good [14, 15]. The procedure doesn't burn any bridges, as it can be revised to a total knee replacement, if ever needed.
|
References
1. Flatow, E.L., et al., Computer simulation of glenohumeral and patellofemoral subluxation. Estimating pathological articular contact. Clin Orthop Relat Res, 1994(306): p. 28-33.
2. Beighton, P., L. Solomon, and C.L. Soskolne, Articular mobility in an African population. Ann Rheum Dis, 1973. 32(5): p. 413-8.
3. Muller, K. and L. Snyder-Mackler, Diagnosis of patellofemoral pain after arthroscopic meniscectomy. J Orthop Sports Phys Ther, 2000. 30(3): p. 138-42.
4. Bolgla, L.A. and M.C. Boling, An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther, 2011. 6(2): p. 112-25.
5. Halbrecht, J.L., Arthroscopic patella realignment: An all-inside technique. Arthroscopy, 2001. 17(9): p. 940-5.
6. Haspl, M., et al., Fully arthroscopic stabilization of the patella. Arthroscopy, 2002. 18(1): p. E2.
7. Prasathaporn, N., S. Kuptniratsaikul, and K. Kongrukgreatiyos, Arthroscopic medial retinacular plication with a needle-hole technique. Arthrosc Tech, 2014. 3(4): p. e483-6.
8. Dickschas, J., et al., Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg, 2012. 132(3): p. 289-98.
9. Leonardi, F., et al., Bilateral double osteotomy in severe torsional malalignment syndrome: 16 years follow-up. J Orthop Traumatol, 2014. 15(2): p. 131-6.
10. Stevens, P.M., et al., Success of torsional correction surgery after failed surgeries for patellofemoral pain and instability. Strategies Trauma Limb Reconstr, 2014. 9(1): p. 5-12.
11. Henrotin, Y., A. Mobasheri, and M. Marty, Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis? Arthritis Res Ther, 2012. 14(1): p. 201.
12. Reginster, J.Y., et al., Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet, 2001. 357(9252): p. 251-6.
13. Jack, C.M., et al., The modified tibial tubercle osteotomy for anterior knee pain due to chondromalacia patellae in adults: A five-year prospective study. Bone Joint Res, 2012. 1(8): p. 167-73.
14. Odumenya, M., et al., The Avon patellofemoral joint replacement: Five-year results from an independent centre. J Bone Joint Surg Br, 2010. 92(1): p. 56-60.
15. Leadbetter, W.B., et al., Patellofemoral arthroplasty: a multi-centre study with minimum 2-year follow-up. Int Orthop, 2009. 33(6): p.1597-601.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |