Frozen Shoulder FAQs
The following article is reviewed by the doctors in Asia Medical Specialists
(Last updated on: September 15th 2020)
What is frozen shoulder?
The term frozen shoulder is ‘abused’ – in other words used casually to describe almost any shoulder pain.
There are many conditions which are often called ‘frozen shoulder’ (including: pain from the neck; shoulder impingement; shoulder tendonitis; and rotator cuff tear; as well as ‘true’ frozen shoulder) even though they are different problems, with different prognoses and treatments, and which should be distinguished from each other.
A common Chinese term which is used and abused in the same way as the English term ‘frozen shoulder’ is ‘50-years-old shoulder’ (五十肩) – essentially meaning shoulder pain in people in middle age. The formal name of ‘true’ frozen shoulder is “adhesive capsulitis”. There
The formal name is “adhesive capsulitis”. There is tightening and thickening of the joint capsule, reducing the range of motion and causing pain. Under the microscope, the appearance of the shoulder joint capsule is very similar to the tissue which stops the fingers from moving in Dupuytren’s contracture [1], a fairly common condition where the little finger curls into the palm.
How common is it?
Common! True frozen shoulder affects about 2% of the general population. It mostly affects people between 40 and 60 years of age, with no clear pattern of sex and arm dominance. It is more common in people with diabetes (up to 20%) and heart disease. Sometimes it follows an injury.
What is it like?
Untreated, the natural history is of three overlapping phases (Frozen stage):
Phase 1: Painful or ‘freezing’ phase
Lasting from 2 to 9 months. There is constant shoulder soreness on movement, and the pain progressively increases. Most have night pain, disturbing sleep. The pain often persists no matter what people do or how they position their arms.
 Fig.1 Painful or ‘freezing’ phase |
Phase 2: Stiffening or ‘frozen’ phase
Lasting from 4 to 12 months. People notice marked stiffening of the shoulder with restriction of movements in all directions. The pain may gradually improve and often only occurs at the extremes of motion. People have difficulty in raising their arms above their own heads, difficult in washing or combing their hair; and women notice difficulty with bras (Fig. 2).
 Fig.2 Women with shoulder stiffness often have difficulty with bra straps |
Phase 3: Resolution or ‘thawing’ phase
Lasting from 1 to 3 years. There is improvement in pain and range of motion. End range pain may still occur until complete recovery. Even after ‘complete’ recovery, there may still be loss of some range of motion, particularly rotation (twisting) and reaching overhead.
Essentially, almost 95% of patients will recover even without treatment, though the whole process averages about 18 months and many will have some loss of range of motion [2].
How should it be diagnosed?
Accurately diagnosing can sometimes be difficult, and the condition is often misdiagnosed, or, more commonly, other conditions are misdiagnosed as ‘frozen shoulder’.
Doctors diagnose frozen shoulder based on the whole picture: the patient’s symptoms and physical examination and the results of imaging and other tests.
In the early phase pain is more prominent than stiffness, and it may be difficult to differentiate it from shoulder impingement syndrome.
Later on, stiffness is more prominent and range of motion is reduced – especially external rotation, and the diagnosis is usually clear.
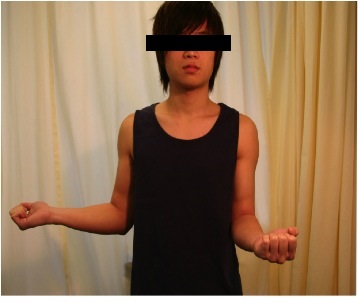
The ‘cardinal sign’ is loss of external rotation (Fig. 3a & 3b). Occasionally, other conditions including posterior dislocation of the shoulder and rotator cuff tears can mimic this problem, so one needs to be a little careful.
Fig.3a Symmetrical external rotation in normal shoulders |
Fig. 3b Loss of external rotation on the left, as would be found in a frozen shoulder |
Other shoulder problems are often confused with frozen shoulder:
- Impingement – there is usually pain but no stiffness and not much weakness. That said, as mentioned above, early frozen shoulder can look like this, and sometimes it is necessary to treat as impingement, with pain relief and physiotherapy, and wait and see.
- Rotator cuff tears – in the early stage there is pain and stiffness, but in the later stages shoulders may be relatively painless and weak.
- Neck problems – usually there is neck pain – though sometimes pressure on a nerve in the neck can cause pain and/or weakness of the shoulder with no or minimal neck pain.
Does X-ray or MRI help?
X-rays and/or MRI are sometimes used to rule out other causes of shoulder stiffness and pain, because frozen shoulder does not really ‘show up’ on imaging. X-ray is taken to exclude shoulder joint dislocations and osteoarthritis (Fig. 4). MRI is used to identify other problems, especially rotator cuff tear, which would require repair. Sometimes MRI shows thickening of the capsule of the shoulder joint.
|
|
Fig. 4 X-ray of a normal shoulder (left) and arthritic shoulder (right) | |
How is frozen shoulder treated?
The goal in treatiment is to achieve improvement in pain and function of the shoulder. A successful treatment is defined individually with the patient in sharing decision making in the treatment process [3]. Frozen shoulder can be treated non-operatively or by operation.
Non-operative treatment helps over 80% of patients, but recovery is often slow.
The principle is to control pain so patients can perform exercises to improve range of motion. Appropriate physiotherapy and close monitoring of progress are mandatory to treatment success. Programmes should be tailored to personal needs so that the patients can return to their daily activities as soon as possible.
Injection of steroids into the shoulder joint can improve pain by reducing the inflammation within the joint. These are quick, relatively painless, and quite safe.
The duration of non-operative treatment can last from a few months to up to 2 years.
Operative treatment
Operative treatment has the advantage of speed – patients usually recover quickly.
It can be offered to patients immediately upon diagnosis or later if they fail to improve with non-operative treatment.
An operation may be particularly beneficial to patients with frozen shoulders related to underlying diabetes, as the failure rate for non-operative treatment is often higher in diabetics.
Operations include manipulations under anaesthesia (MUA) and arthroscopic capsular release. These two procedures can be performed at the same time.
MUA was the earliest form of treatment. It consists of gently but firmly forcing the shoulder through a complete range of motion, thus tearing the tight capsule. It works well, but the shoulder is painful for about 10 weeks after the procedure [4].
The modern standard of care is arthroscopic capsular release operation - a minimally-invasive arthroscopic procedure to cut (rather than tear) the capsule. This is much less painful than MUA, and patients usually virtually fully recover in a few weeks [5]. It is also quite safe, with <1% risk of significant complications such as nerve injuries and broken bones.
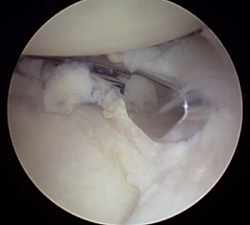 |
|
Fig. 5 Arthroscopic scissors cutting the anterior capsule (right) and after release (left) | |
It is important to keep the shoulder moving after the capsular release, or the shoulder will stiffen up again. This requires good pain control and regular physiotherapy and home exercises. Recovery time after surgery varies from about 1 to 3 months.
The long-term outcomes are generally good with the majority of the patients having reduced or no pain, and increased range of motions. However, in a small percentage of cases, there may still be mild residual stiffness despite physiotherapy.
Are there any other treatments?
Because it is common, many treatments have been tried. With the exception of the treatments described above, none have been proven to be effective.
In particular ‘hydrodilatation’ - injecting anaesthetic and/or other liquids into the shoulder joint under pressure to try to increase its volume has been shown to be ineffective. The fluid bursts out of the weakest place in the joint without affecting the joint overall. A good study comparing hydrodilatation with steroids to steroid injection alone showed no difference in outcome [6].
Are steroid injections safe?
In Hong Kong, there is great concern about the risks and side-effects of steroids. Steroids are powerful drugs, which, used appropriately, can be very helpful, but, used inappropriately, can cause problems. In general, we limit steroid injections to a maximum of three per joint - if a patient is not better after three injections they are unlikely to get better with further injections. Repeated injections risk damaging the rotator cuff tendons. The risks of any injection include infection, but this is a very very rare complication. The majority of the steroid stays locally and does not cause generalised steroid side effects, though diabetics may notice their blood sugar control is affected by the injection. So in summary, used appropriately, steroids are ‘safe’.
References
1. Ozaki, J., et al., Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am, 1989. 71(10): p. 1511-5.
2. Vastamaki, H., J. Kettunen, and M. Vastamaki, The natural history of idiopathic frozen shoulder: a 2- to 27-year followup study. Clin Orthop Relat Res, 2012. 470(4): p. 1133-43.
3. Rangan, A., et al., Frozen Shoulder. Shoulder Elbow, 2015. 7(4): p. 299-307.
4. Charnley, J., Periarthritis of the shoulder. Postgrad Med J, 1959. 35: p. 384-8.
5. Ogilvie-Harris, D.J., et al., The resistant frozen shoulder. Manipulation versus arthroscopic release. Clin Orthop Relat Res, 1995(319): p. 238-48.
6. Tveitå, E.K., et al., Hydrodilatation, corticosteroids and adhesive capsulitis: A randomized controlled trial. BMC Musculoskeletal Disorders 2008, 9:53
Articles written/edited/reviewed by Doctors of Asia Medical Specialists ©2018 Asia Medical Specialists Limited. All rights reserved. |