ACL FAQs
ACL FAQs
Written By Dr Chi-Chong KONG
(Last updated on: Oct 13th 2020)
You are sprinting down the wing, a defender comes for you, you cut inside, but as you push off your knee goes 'pop' and you fall over in agony. You are helped off the field and watch your team win (without you!) with a bag of ice on your knee. After the game your knee feels a bit better, and you join your teammates for a celebratory drink, and when you get home, you feel fine. The next morning your knee is agony! You limp to the doctor, who does an X-ray and tells you the bones are fine. Over the next few weeks your knee gets better, and you are soon back on the pitch – dashing up the wing … you cut inside a defender… and end up face down….
Does this story sound familiar? It is typical of an ACL tear.
What is the ACL?
How does the ACL get torn?
 Fig. 1 Two bundles in normal anterior cruciate ligament |
 Fig. 2 Ruptured Anterior Cruciate Ligament |
What will happen to my knee if my ACL is torn?
How do I know if my ACL is torn?
 Fig. 3 MRI from Shanghai shows intact ACL marked by arrows. |
What should I do if my ACL is torn?
Is ACL surgery absolutely necessary?
What about bracing?
Are there any age limits for ACL reconstruction?
Older people need ACL reconstruction if their knee instability is a problem [7,8]. The oldest person reported in the medical literature to have an ACL reconstruction was a rancher who could not work normally because his knee was unstable. He was 84 [9].
What does ACL reconstruction involve?
What is the surgical technique?
 Fig. 4 Arthroscopic view during ACL reconstruction showing how the two bundles of the ACL cross |
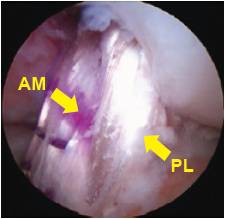 Fig. 5 Reconstructed two bundles of anterior cruciate ligament |
Why double-bundle, instead of single-bundle?
On long term follow-up after single bundle ACL reconstruction, 10-30% patients complain of knee pain and residual instability, while arthritis has been observed on X-rays in up to 90% of patients [13,14].
Biomechanical studies of double-bundle ACL reconstruction have shown superior rotational stability to single-bundle ACL reconstruction [15].
It is very likely that the improved short-term results will be maintained in the long-term.
What can I expect after ACL reconstruction?
References
1. Anstey DE, Heyworth BE, Price MD, Gill TJ. (2012). "Effect of timing of ACL reconstruction in surgery and development of meniscal and chondral lesions." Phys Sportsmed Feb;40(1):36-40.
2. Guillodo Y, Rannou N, Dubrana F, Lefevre C, Saraux A. (2008). "Diagnosis of anterior cruciate ligament rupture in an emergency department." J Trauma Nov;65(5):1078-82.
3. Fetto JF, Marshall JL. (1979). "Injury to the anterior cruciate ligament producing the pivot shift sign." JBJS Am Jul;61(5):710-4.
4. Leitze Z, Losee RE, Joki P, Johnson TR, Feagin JA. (2005) "Implications of the pivot shift in the ACL-deficient knee." CORR Jul;(436):229-36.
5. Yoon KH, Yoo JH, Kim KI. (2011).”Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture.” J Bone Joint Surg Am. Aug 17;93(16):1510-8.
6. B. Swirtun LR, Jansson A, Renstrom P. (2005). “The effect of functional knee brace during early treatment of patients with a non-operated acute ACL tear: a prospective randomized study.” Clin J Sport Med. Sept; 15(5):299-304.
7. Arbuthnot JE, Brink RB. (2010). “The role of anterior cruciate ligament reconstruction in the older patients, 55 years or above.” Knee surg Sports Traumatol Arthrosc. Vol 18, Number 1,73-78.
8. Osti L, Papalia R, Del Buono A, Leonardi F, Denaro V, Maffulli N. (2011). “Surgery for ACL deficiency in patients over 50.” Knee Surg Sports Traumatol Arthrosc. Mar; 19(3):412-7.
9. Miller MD, Sullivan RT. (2001). “Anterior cruciate ligament reconstruction in an 84-year-old man.” Arthroscopy Jan;17(1):70-2.
10. D. Leis HT, Sanders TG, Larsen KM, Lancaster-Weiss KJ, Miller MD. (2003). “Hamstring regrowth following harvesting for ACL reconstruction: The lizard tail phenomenon.” J Knee Surg. Jul; 16(3):159-64.
11. Tashman S, C. D., Anderson K (2004). “Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction.” Am J Sports Med 32: 975-983
12. Yagi M, W. E., Kanamori A. (2002). “Biomechanical Analysis of an Anatomical Anterior Cruciate Ligament Reconstruction.” Am J Sports Med 30: 660-666
13. Anderson AF, S. R., Lipscomb AB Jr (2001). “Anterior cruciate ligament reconstruction. A prospective randomized study of 3 surgical methods. .” Am J Sports Med(29): 272-279
14. Fithian DC, P. E., Stone ML (2005). “Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee.” Am J Sports Med 33(3): 333-334.
15. Hemmerich A, van der Merwe W, Batterham M, Vaughan CL. (2011). “Double-bundle ACL surgery demostrates superior rotational kinematics to single-bundle technique during dynamic task.” Clin Biomech (Bristol, Avon). Dec; 26(10):998-1004.
16. Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. (2008). “Prospective clinical comparisons of anatomic double- bundle versus single-bundle ACL reconstruction procedures in 328 consecutive patients.” Am J Sports Med. Sept;36(9):1675-87.
17. Jarvela T. (2007). “Double bundle versus single-bundle ACL reconstruction: a prospective randomize clinical study.” Knee Surg Sports Taumatol Arthrosc. May;15(5):500-7.
18. Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK. (2009). “Prospective comparative study of ACL reconstruction using the double-bundle and single-bundle techniques.” Am J Sports Med. Sep;37(9):1705-11.
| Copyright ©2017 Asia Medical Specialists Limited. All rights reserved. |
